Obesity
Obesity 1
393 - Prenatal Starting Early Program to Promote Healthy Nutrition, Lifestyle and Growth during Pregnancy and Infancy: Findings from a Single Arm Feasibility Study
Publication Number: 393.145

Mary Jo Messito, MD (she/her/hers)
Clinical Associate Professor
New York University Grossman School of Medicine
New York, New York, United States
Presenting Author(s)
Background:
US pregnant women have high rates of suboptimal diet and activity, and adverse social determinants of health (SDoH), leading to obesity related co-morbidities. The Starting Early Program (StEP) is a dietitian-delivered supportive intervention spanning pregnancy and infancy designed to promote healthy nutrition and lifestyle. The original StEP RCT was one of the first obesity prevention trials spanning from the 3rd trimester through infancy. Latina mother-infant pairs with low income who participated in StEP had improved diet, lifestyle and child weight. StEP Prenatal extends this approach to the 1st trimester.
Objective:
To assess diet, activity, and SDoH outcomes among Latina mother-infant pairs participating in StEP Prenatal from the 1st trimester of pregnancy through infant age 19 months.
Design/Methods:
A single arm longitudinal trial enrolled pregnant women in the 1st trimester to receive StEP Prenatal (8 prenatal and 11 pediatric nutrition and parenting support sessions). Diet and activity (e.g., vegetable intake, screen time) and SDoH (e.g., food insecurity, depression) were collected with validated surveys. Gestational weight gain was collected from the medical record. Two comparisons were conducted: 1) within the single arm trial (n=238): pre- and post-intervention comparisons of 1st vs. 3rd trimester assessments using paired t-tests; and 2) between 3rd trimester assessments of StEP Prenatal and original StEP RCT (n=533) using linear and logistic regression.
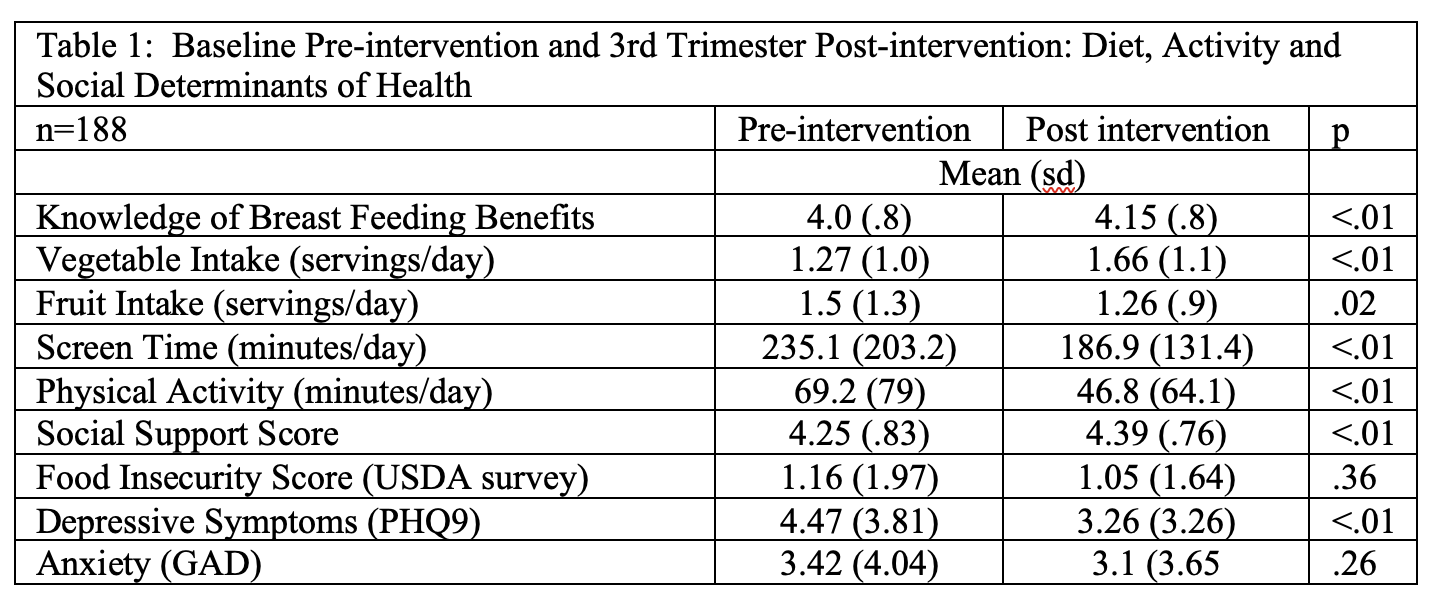
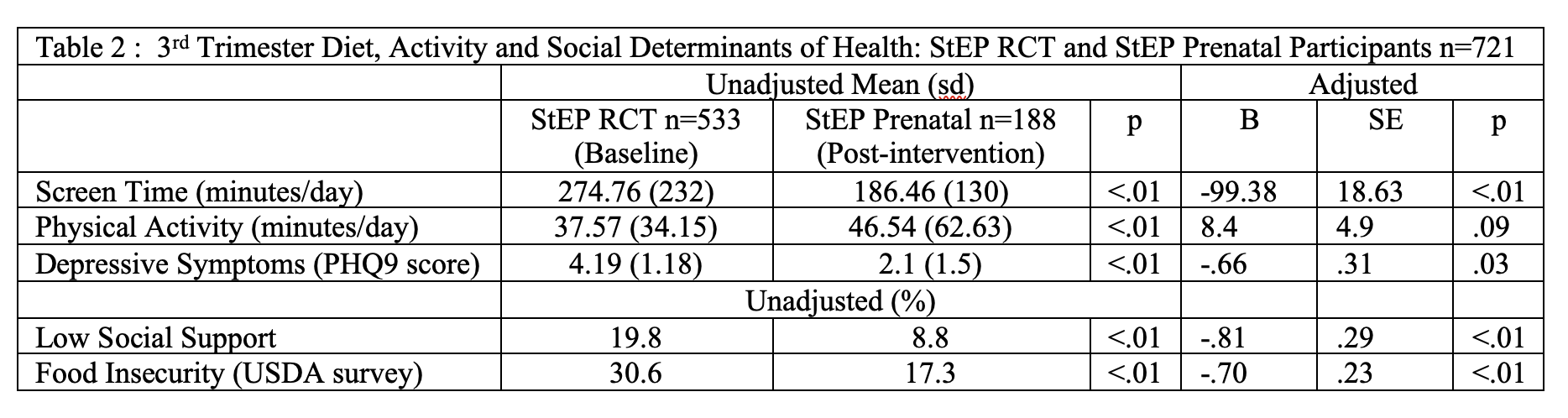
Results: 238 1st trimester women enrolled into the StEP Prenatal cohort, with 24 pregnancy losses. Baseline and 3rd trimester data available for 188. Mean maternal age 28.5 years, mean prepregnancy BMI 28.8, 23.6% had < HS education, 70.3% lived with partner, 24.9% US Born, 40.9% primiparous, 73.3% received WIC and 24.6% SNAP. The median attendance was 7 prenatal and 8 pediatric sessions. In pre- and post-intervention analyses, vegetable intake, knowledge of breastfeeding benefits and screen time improved between 1st and 3rd trimesters; rates of low social support, food insecurity and depressive symptoms decreased (Table 1). Compared to StEP RCT participants, StEP Prenatal participants had lower rates of food insecurity, low social support, depressive symptoms and screen time, and higher physical activity (Table 2).
Conclusion(s): Attendance at a supportive intervention spanning pregnancy and infancy was high and associated with improvements in key diet and lifestyle behaviors, and SDoH. Findings highlight the additive effects of intervention in early pregnancy to enhance two-generational impacts and support the need for further study.