Obesity
Obesity 2
406 - Social determinants of health and engagement in an early child obesity prevention program beginning in pregnancy, for Latinx families with low income.
Publication Number: 406.146

Michelle W. Katzow, MD, MS (she/her/hers)
Assistant Professor
Feinstein Institutes for Medical Research, Cohen Children's Medical Center
Cohen Children's Medical Center
New Hyde Park, New York, United States
Presenting Author(s)
Background:
Efficacy of early child obesity prevention programs is limited by poor program engagement, but literature is mixed regarding the effects of social determinants of health (SDoH) on program engagement.
Objective:
To determine: 1) associations between two domains of SDoH (mental health symptoms and material hardships) and engagement in an early child obesity prevention program, beginning in the first trimester of pregnancy and continuing to child age 18 months; and 2) if associations between SDoH and program engagement vary by baseline social support.
Design/Methods:
Starting Early Prenatal, a single arm trial of a group-based, supportive intervention, designed to prevent child obesity in low-income, Latinx families, consisted of 8 prenatal and 9 postnatal sessions. We used zero inflated Poisson regression to test associations between baseline SDoH (mental health symptoms: stress, depression, anxiety; material hardships: food insecurity, unsafe neighborhood, financial distress, housing insecurity, housing disrepair) and program engagement (number of missed sessions). We used interaction terms to test for moderation by baseline social support and adjusted for maternal age, marital status, nativity, and education.
Results:
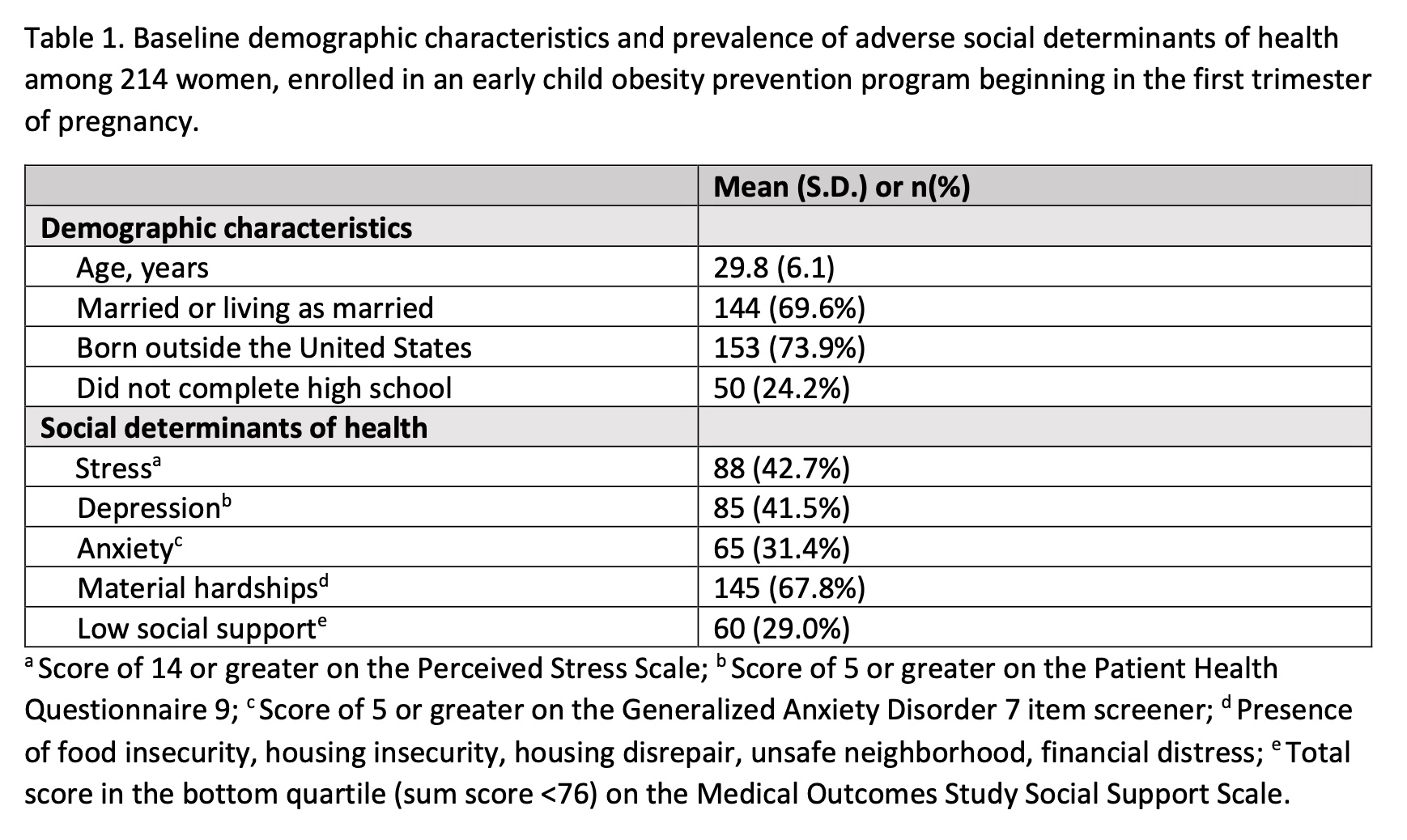
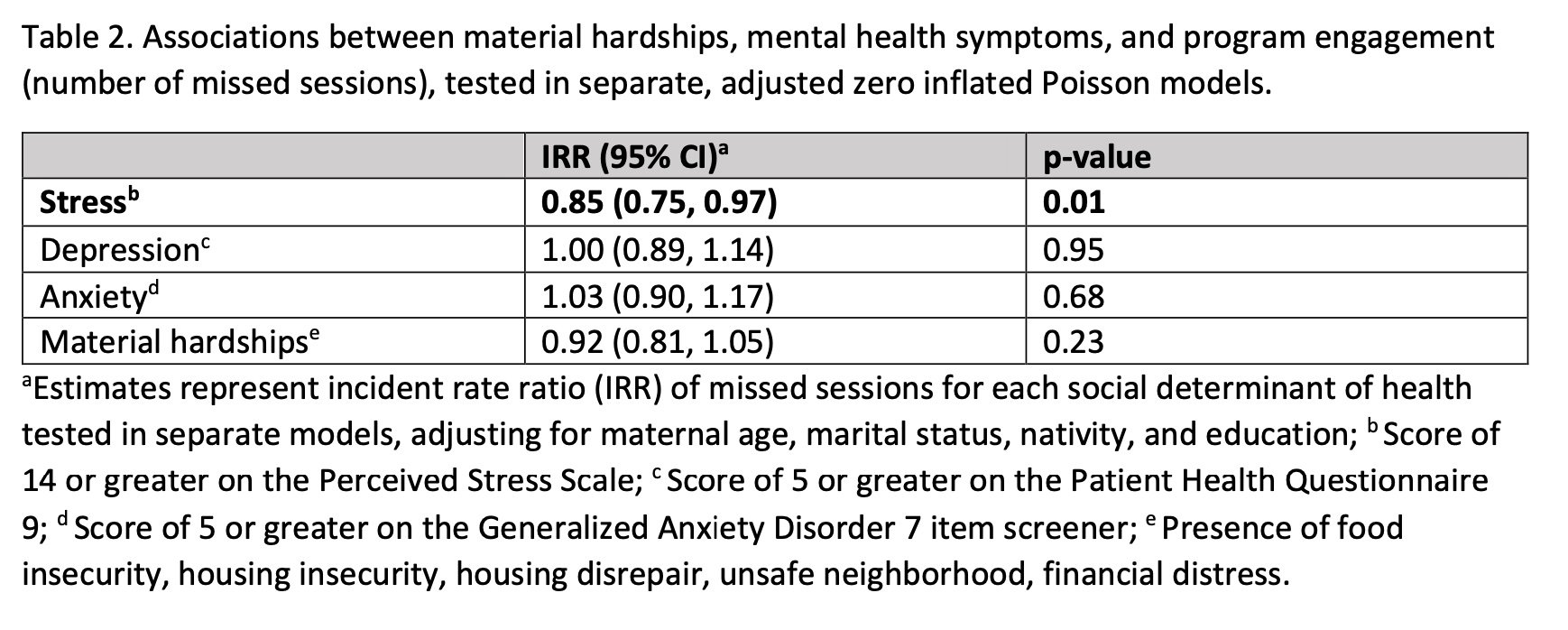
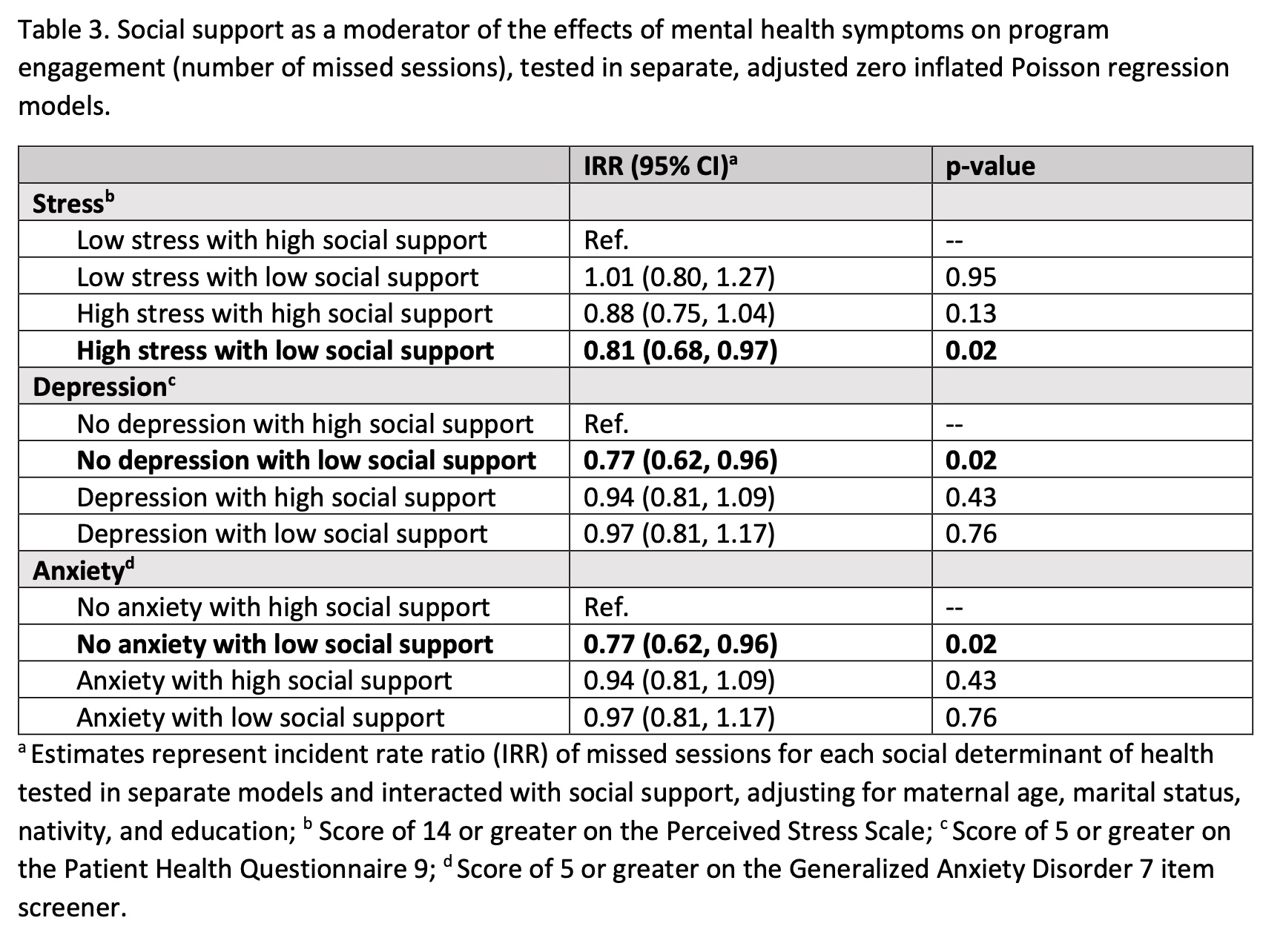
There were 214 women eligible to receive the 17-session program. Median (IQR) number of missed sessions was 4 (1,9). Demographic characteristics and prevalence of adverse SDoH are shown in Table 1. Symptoms of stress were significantly associated with 15% higher program engagement (incidence rate ratio [IRR]=0.85, p=0.01), compared to no stress. There were no significant associations between symptoms of depression, anxiety, or presence of material hardships and program engagement (Table 2). In moderation analyses (Table 3), stress was significantly associated with 19% higher engagement among those with low social support (IRR=0.81, p=0.02; compared to no stress with high social support). Low social support was also significantly associated with higher engagement in those without symptoms of depression (IRR=0.77, p=0.02) or anxiety (IRR=0.73, p< 0.01) compared to high social support and no symptoms of depression or anxiety, respectively.
Conclusion(s):
Latina women with low social support early in pregnancy may be particularly motivated to engage in a supportive, group-based child obesity prevention program if they are also experiencing symptoms of stress, but not if they are experiencing symptoms of depression or anxiety. Programs should consider tailoring their implementation models to baseline mental health symptoms and social support.