Clinical Bioethics
Clinical Bioethics 1
420 - Validation of a Process for Shared Decision-Making in Pediatrics
Publication Number: 420.106
.jpg)
Holly H. Vo, MD, MPH, MSc, MA (she/her/hers)
Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background:
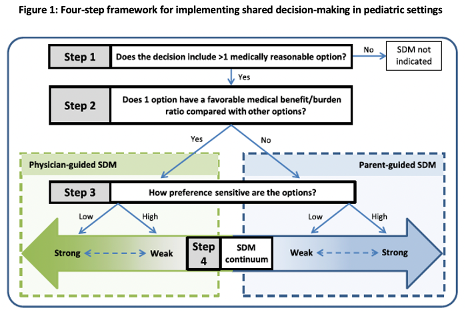
Background: Implementation of shared decision-making (SDM) and measurement of its impact on health care quality are key national priorities. However, the concept and process of SDM in pediatrics remains poorly understood. We previously conceptualized a best practice, 4-step process for implementing SDM in pediatric settings (Figure 1).
Objective:
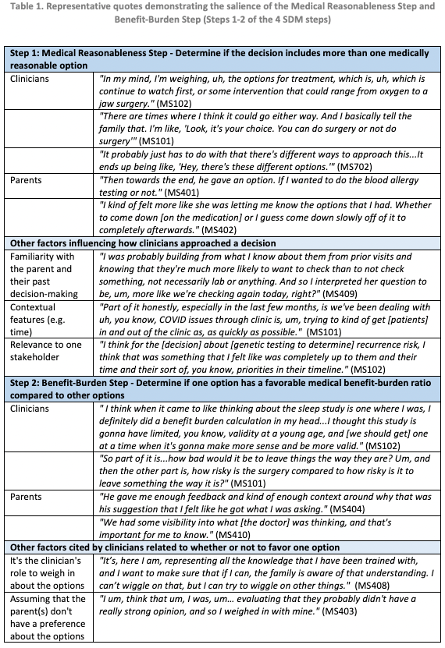
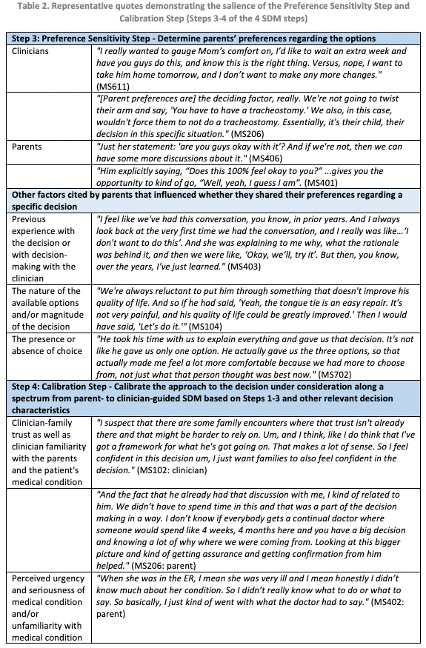
Objective: To confirm, refute, or modify our previously developed 4-step pediatric SDM process that involves: 1) determining if the decision includes >1 medically reasonable option; 2) determining if 1 option has a favorable medical benefit-burden ratio compared to other options; 3) determining parents' preferences regarding the options; and 4) calibrating the SDM approach based on other relevant decision characteristics (Figure 1).
Design/Methods:
Methods: We videotaped a purposive sample of pediatric inpatient and outpatient encounters at a single US children's hospital. Clinicians from 7 clinical services (craniofacial, hospital medicine, neonatology, oncology, pediatric intensive care, pulmonary, and sports medicine) were eligible. English-speaking parents of children who participated in inpatient family care conferences or outpatient problem-oriented encounters with participating clinicians were eligible. We conducted individual post-encounter interviews with clinician and parent participants utilizing video-stimulated recall to facilitate reflection of decision-making that occurred during the encounter. We utilized direct content analysis with open coding of interview transcripts to determine the salience of the 4-step SDM process and identify themes that confirmed, refuted, or modified this process.
Results:
Results: We videotaped 30 encounters with ≥1 videotaped encounter from each clinical service. We conducted 53 post-encounter interviews of parent and clinician participants: 25 with parents and 28 with clinicians (23 unique clinicians, with 5 clinicians contributing 2 interviews each). We found that clinicians' and parents' experiences of decision-making confirmed each SDM step (Tables 1 and 2). However, there was variation in the interpretation of each step and a need for flexibility in implementing the process depending on specific decisional contexts.
Conclusion(s):
Conclusions: In this observational study, we identified themes that support a 4-step process for implementing SDM across a range of decision-making scenarios in pediatrics. The 4-step SDM process for pediatrics appears to be salient and may benefit from further guidance about the interpretation of each step and contextual factors that support a modified approach.