Hospital Medicine: Newborn Care
Hospital Medicine 2
769 - Reducing Laboratory Testing and Blood Draws in the Newborn Nursery to Increase High-Value Care
Publication Number: 769.12

Lauren Z. Foster, MD (she/her/hers)
Assistant Professor
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background:
Newborn infants are often subjected to multiple blood tests prior to hospital discharge, some of which are unnecessary and due to outdated hospital policies and provider variability. Such tests also cause pain, which is compounded by multiple skin punctures. Reducing unnecessary laboratory testing in alignment with evidence-based guidelines can improve the value (quality/cost) of healthcare, and clustering of blood sampling can reduce pain. We initiated a quality improvement project to accomplish these goals.
Objective:
To reduce the weekly number of blood draw skin punctures and laboratory tests per patient day for newborns in the nursery by 10% by December 2022.
Design/Methods:
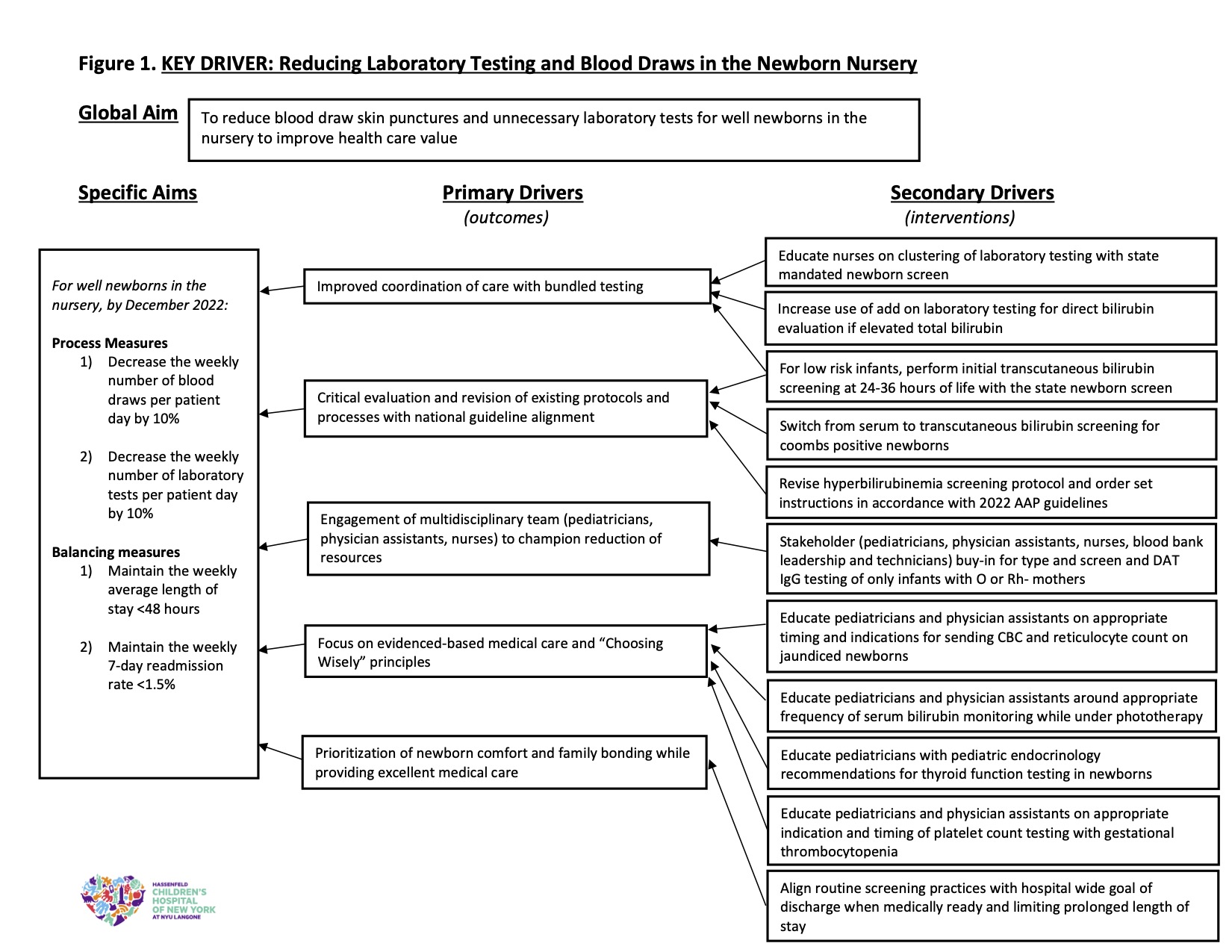
We convened a multidisciplinary team of pediatric attendings, physician assistants (PA) and nurses (RN) to develop and address key drivers (Fig 1). We used the Model for Improvement and Plan-Do-Study-Act cycles. Interventions included education of physicians, PA and RN on clustering of laboratory tests with the state-mandated newborn metabolic screen, “Choosing Wisely” principles, and the newly revised AAP hyperbilirubinemia clinical guidelines. All common blood tests were included, except bedside glucose testing, which was performed based on hospital protocol without opportunity for modification. Any blood tests collected with the required newborn metabolic screen were not counted as a blood draw. Our balancing measures were to maintain 1) average length of stay (LOS) < 48 hours and 2) 7-day readmission rate < 1.5%. Data were collected using electronic health record reports from 9/2021-11/2022 and analyzed with statistical process control (SPC) charts.
Results:
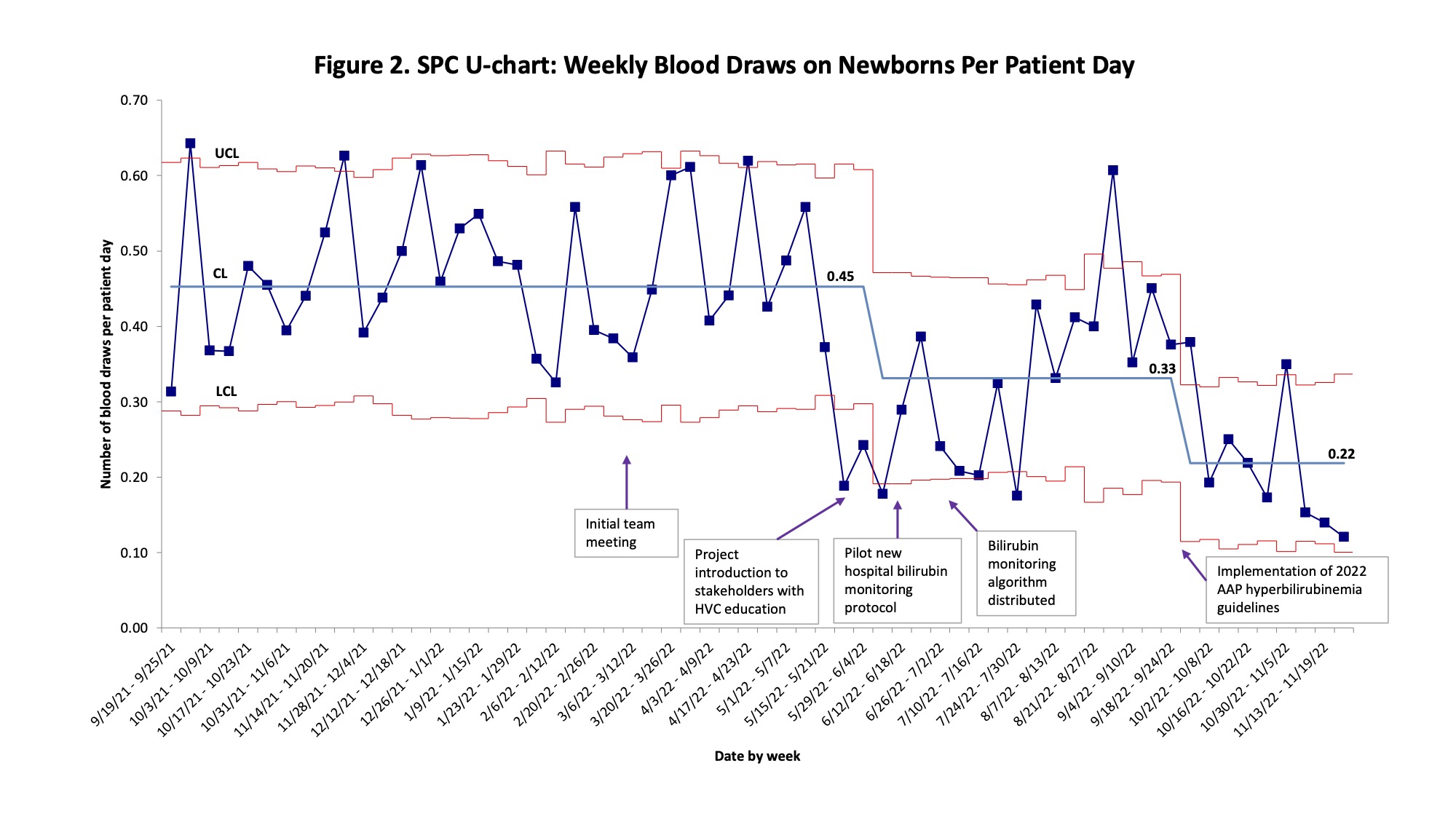
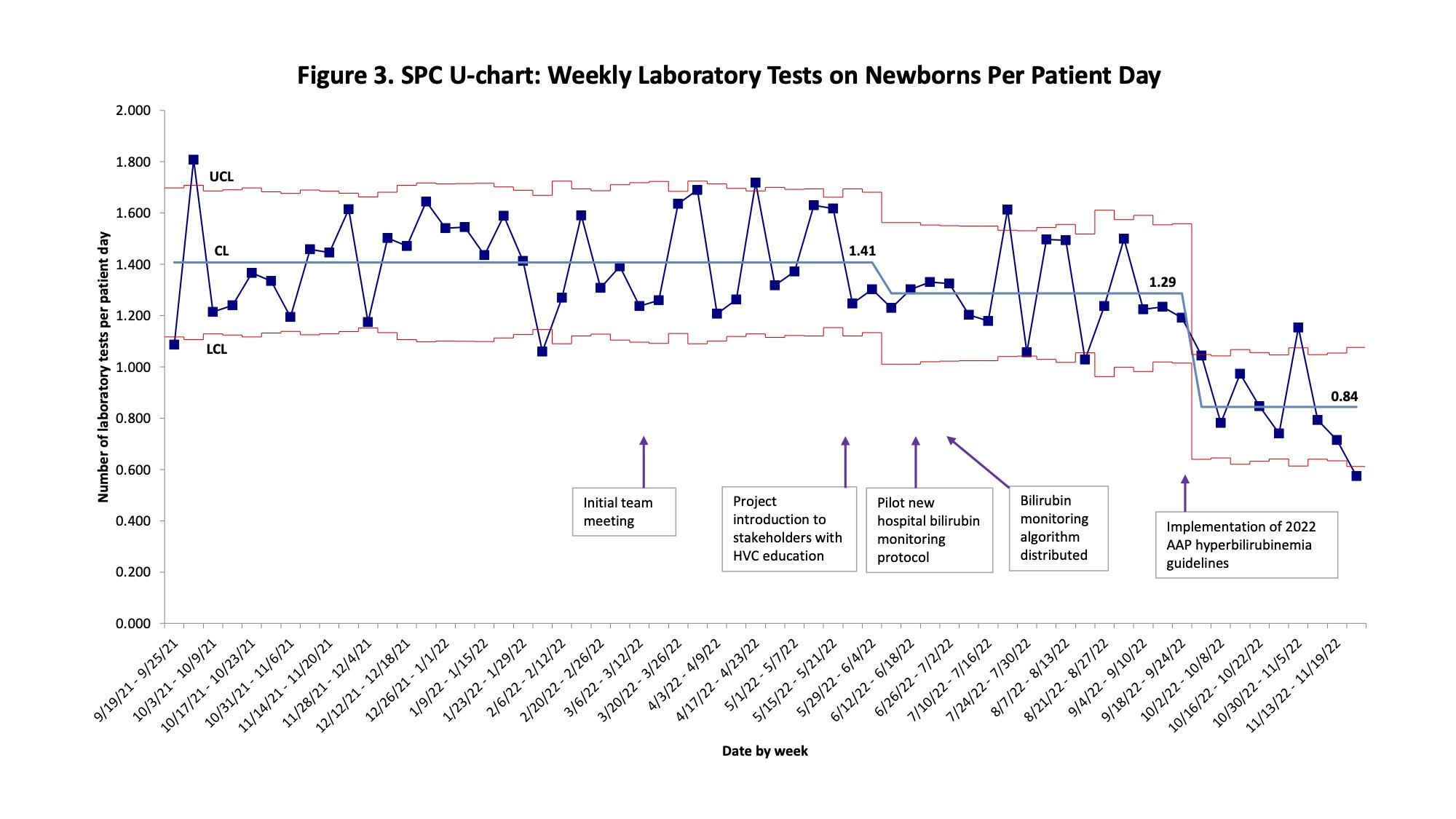
We included 5197 patients admitted to the well newborn nursery over 15 months. The SPC U-chart of blood draws per patient day had a centerline shift from 0.45 to 0.33 after educational interventions, with a decrease to 0.22 after implementation of the revised hyperbilirubinemia clinical guidelines, a 50% decrease (Fig 2). Analysis of laboratory tests per patient day showed similar shifts from 1.41 to 1.29 to 0.84, a 40% decrease (Fig 3). Average LOS increased to 50.7 hours associated with unrelated hospital changes. There was no change in readmission rates.
Conclusion(s):
We achieved substantial decreases in blood draw skin punctures and laboratory tests performed on well newborns, thereby increasing value and decreasing pain, without any adverse effects. Further investigation is needed into outlier weeks, which may be due to patient characteristics or ordering provider variability. Selective newborn blood type testing is an additional opportunity for improvement.