Clinical Bioethics
Clinical Bioethics 1
413 - Ethical Challenges of Pediatric Medical Complexity: Family Perspectives
Publication Number: 413.106
- MS
Miriam C. Shapiro, MD (she/her/hers)
Assistant Professor, Pediatrics
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background:
Medical advances and technologies are helping children with serious illness live longer and better; yet for some children serious illness persists. Caregivers of children with serious illness sometimes need to make difficult decisions, often ones with ethical dimensions. These ethical tension points weigh heavily on families and clinicians. While clinicians can access a variety of ethics supports including ethics experts and literature, these resources are less available and accessible to families.
Objective:
To explore ethical tensions families encounter in their child’s medical care and where those tensions arise.
Design/Methods:
Families of children with medical complexity completed a web-based survey in Fall 2022. Surveys were distributed via family advocacy groups. The survey sought to measure family respondents’ experiences with specific ethically challenging situations in the care of their child with medical complexity and whether their ethical concerns persisted. Respondents also reported their demographics, educational backgrounds, financial resources, and their child’s medical needs.
Results:
We received 205 completed surveys. Caregiver demographics are described in Table 1. Caregivers reported if they had experienced tension points in the care of their child (Table 2). Tension points most frequently identified by caregivers pertained to decisions about letting their child participate in school, sports, or social activities; disagreements with the medical team about the best choice of treatment; and concerns about pain treatment. The most common persistently distressing tension points for caregivers occurred: when they worried the medical team was biased against the child or family; when they worried the medical team was withholding information; when they were not sure how to use an advance directive to plan for care; and when the child was seriously ill and there was a question about life sustaining treatments. Many ethical tensions identified by caregivers pertained to caregiver-child interactions.
Conclusion(s):
Ethical tensions are common for caregivers of children with medical complexity and many leave residual distress. Tensions most frequently identified by our respondents have limited overlap with those most commonly addressed in the ethics literature pertaining to children with medical complexity and clinicians may be less attentive to those tensions that arise over caregiver-child interactions. To optimally support families through decisions for their children, we need to understand their ethical concerns and ensure that adequate resources are available.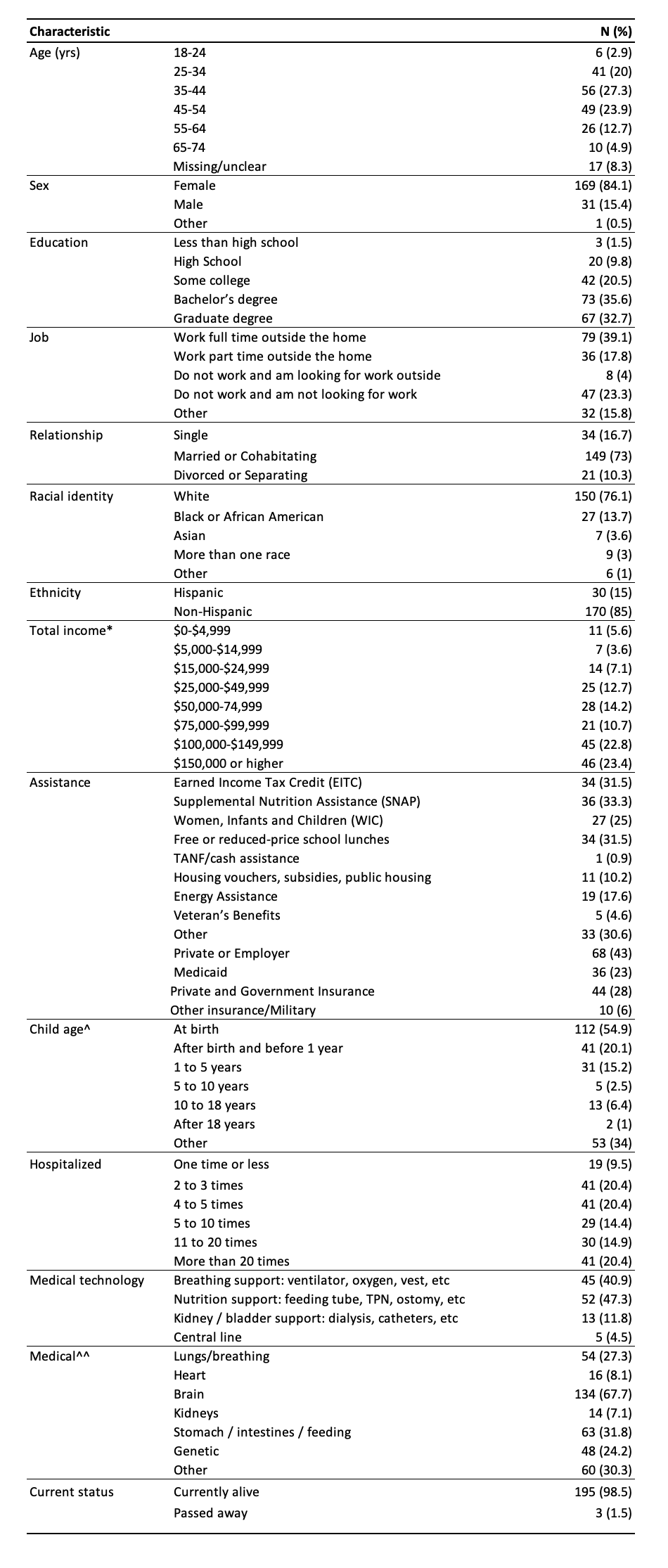
.png)
