Clinical Bioethics
Clinical Bioethics 1
417 - Periviability: What Makes a Unit Culture?
Publication Number: 417.106

Shannon Y. Adams, MD (she/her/hers)
Resident
Lurie Children's Hospital
Chicago, Illinois, United States
Presenting Author(s)
Background:
Research has demonstrated associations between organizational culture and healthcare outcomes. However, the “culture” of an individual medical unit is often difficult to define. This is particularly relevant in the NICU for infants born in the periviable period between 22 and < 25 weeks gestation. Significant institutional variability exists in clinical practice for this patient population – from maternal counseling and obstetric intervention to initial resuscitation measures and ongoing treatment approaches – and this variability leaves room for influence from unit “culture”: how the unit functions, how teams within it choose to care for periviable patients, and how team members feel about and experience the work they do.
When considering how to improve care for extremely preterm neonates, it becomes relevant to examine what constitutes unit “culture,” and whether it can be modified over time.
Objective: To define the core components of a NICU unit’s culture around/attitudes toward the care of infants born during the periviable period.
Design/Methods:
Qualitative, semi structured interviews were conducted at a large Midwestern hospital with members from six clinical groups identified as providers with a key role in the care of periviable infants and their families. Audio recordings were obtained and analyzed with NVivo software for thematic patterns, including frequency, intensity, specificity, and participant perception of importance.
Results:
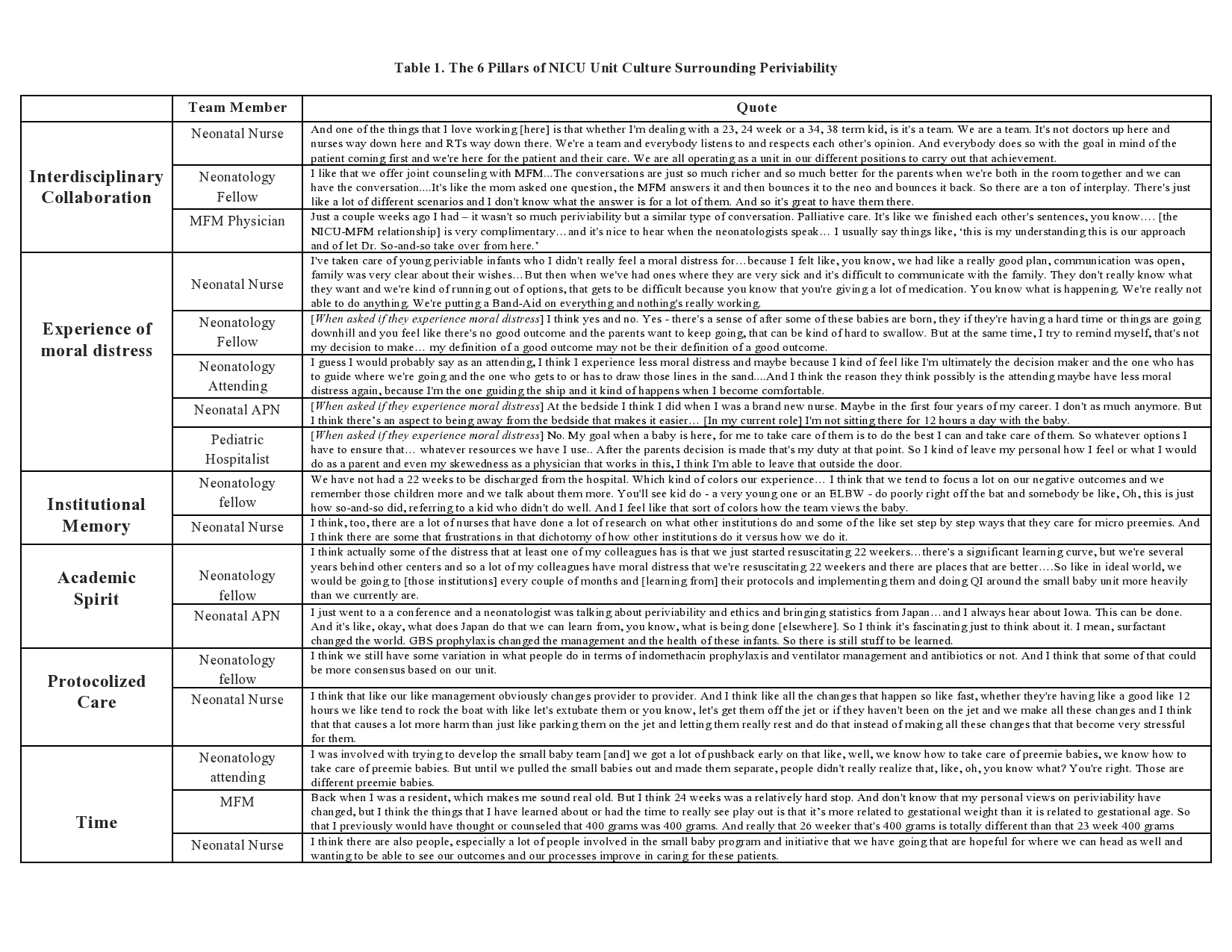
22 interviews were conducted with 5 attending neonatologists, 5 neonatal-perinatal fellows, 3 maternal fetal medicine physicians, 3 neonatal bedside nurses, 3 neonatal advanced practice nurses, and 3 pediatric-NICU hospitalists. Respiratory therapists were invited but unable to participate. Thematic analysis revealed six core pillars that characterize neonatal unit culture towards periviable infants (Table 1): interdisciplinary collaboration, experience of moral distress, institutional memory, academic spirit, protocolized care, and time. Interview participants also suggested specific practices which they felt could modify current culture.
Conclusion(s):
Though it can be challenging to define the specific culture of a unit, particularly regarding a topic as nuanced and complex as periviability, unifying motifs exist. These can potentially be targeted to better understand their unique influence on and across individual centers. Exploration of a unit’s local culture may attune providers to shared opportunities and decrease moral distress, which could ultimately lead to improvements in patient care.