Neonatal Fetal Nutrition & Metabolism
Neonatal GI Physiology & NEC 4: Gut Health, Enteral Nutrition and Oral Feeding
89 - Evaluating the Effect of Infant Gestational Age (GA) on a Standardized Cue-Based Feeding (CBF) Protocol in Preterm Infants (PTI)
Publication Number: 89.236

Isabelle M. Moore, BS (she/her/hers)
Medical Student, MS3
University of Connecticut School of Medicine
Bloomfield, Connecticut, United States
Presenting Author(s)
Background:
The achievement of sufficient oral feeds is a competency that determines the timing of PTI discharge from the NICU. CBF focuses on developmental cues and feeding quality rather than quantity. Evidence shows that infants achieve full oral feeding earlier with CBF than those fed with volume driven methods, but few studies have evaluated oral feeding outcomes using this protocol. GA is a major predictor of NICU outcomes. Thus we have hypothesized that infant GA will affect time to full oral feeds in premature infants.
Objective:
To determine the impact of GA on the achievement of full oral feeds in premature infants born at 23-31 wks. GA, using a standardized CBF protocol.
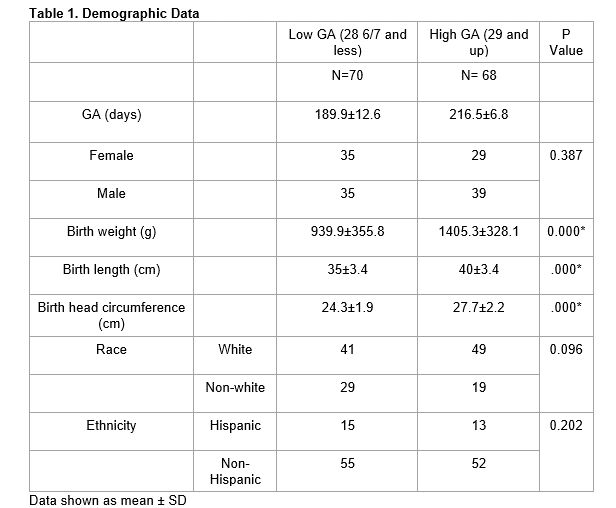
Design/Methods: A retrospective study was conducted at Connecticut Children’s NICU at UConn Health in Farmington, CT from CBF implementation in Jan 2017 to Mar 2021. Feeding data was collected through chart review. Inclusion criteria consisted of infants between 23 wks. and 31 wks. GA. Infants transferred out of the NICU before reaching full oral feeds (140cc/k/day), transferred in after starting a non-CBF protocol, infants with NEC, and infants with genetic, GI, congenital heart or neurological abnormalities were excluded due to impact on feeding velocity. Potential confounders including BPD, BW, RDS, PDA, IVH, ROP, and GERD were included in the analysis. Two-tailed unpaired t-tests, chi-squared test and multiple linear regression (MLR) were used for data analysis.
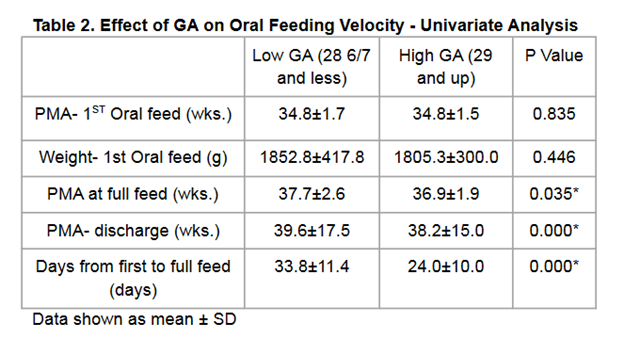
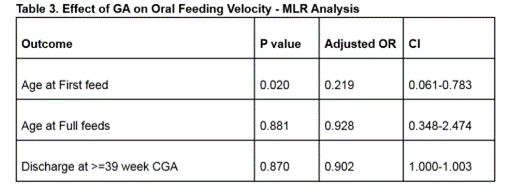
Results: (See Table 1., Table 2., Table 3.) Data from 138 infants (low GA group (LGA) n=70 and high GA group (HGA) n=68) were included. HGA attained full feeds and were discharged at significantly earlier postmenstrual age (PMA) than LGA. HGA also had significantly shorter duration between first and full oral feeds than LGA . After adjusting for BPD, GERD and birth weight (potential confounders) there was no significant difference in PMA at full feeds or discharge for the GA groups. However, after adjusting for the same confounders, there was significantly earlier first feed initiation in HGA.
Conclusion(s): Use of a standardized CBF protocol in the NICU demonstrated that HGA infants achieved earlier achievement of full oral feeds and discharge than LGA infants. Additionally, HGA infants also had a shorter duration between first and full oral feeds. Adjustment for potential confounders demonstrated HGA infants achieved first oral feeds earlier than LGA although the difference in achievement of full feeds and discharge between GA groups did not remain significant. We plan to conduct further analysis to examine factors affecting oral feeding velocity using the CBF protocol.