Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 2
234 - Outcomes Associated with Early vs. Late Acute Kidney in Extremely Low Birthweight Neonates with Patent Ductus Arteriosus
Publication Number: 234.243
- DS
David Selewski, MD, MSCR
Associated Professor
Medical University of South Carolina
Mount Pleasant, South Carolina, United States
Presenting Author(s)
Background: In neonates little is known about how the timing of acute kidney injury (AKI) development impacts outcomes. Furthermore, the impact of patent ductus arteriosus (PDA) status on associations between AKI and outcomes could be considerable but remains understudied.
Objective: We aimed to determine if outcomes differed between neonates with early (i.e. within the first week of life), late (i.e. beyond the first week of life), or both early and late AKI and if PDA status impacted these associations.
Design/Methods:
Single center retrospective cohort study of neonates < 28 weeks gestational age (GA) and < 1,000 grams at birth (i.e., extremely low birth weight, ELBW) admitted 3/15/16-3/14/22 with PDA. Exclusion criteria: admission to our center at >12 hours of life, ductal-dependent cardiac disease, palliative course pursued within first 7 days of life, death before day of life 8.
Associations between AKI groups and both length of stay (LOS) and mortality were examined using bivariate and multivariate linear and logistic regression models, respectively, adjusted for receipt/non-receipt of indomethacin PDA prophylaxis (ppx) and PDA status.
Results:
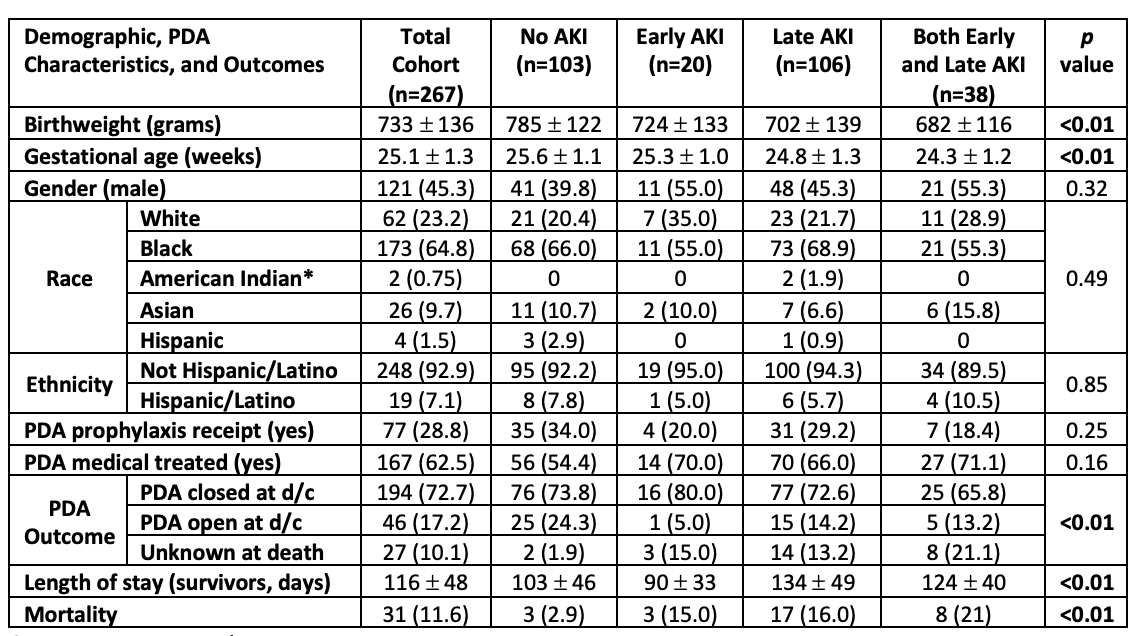
Of 267 neonates included, 20 (7.5%) developed early AKI, 106 (39.7%) developed late AKI, and 38 (14%) developed both early and late AKI. Mean LOS was 116 ± 48 days, and 236 (88%) neonates survived to discharge. Neonates with early, late, and both early and late AKI had progressively lower birthweights and GA’s, respectively, however race, ethnicity, ppx receipt, and PDA medical treatment receipt did not differ between groups. PDA outcomes varied by AKI status however most neonates had closed PDA at discharge (Table 1).
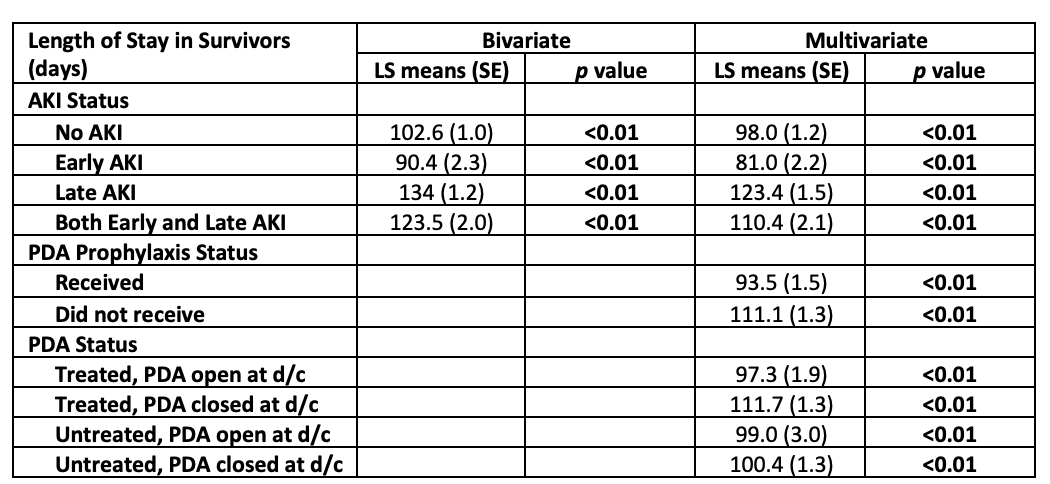
Those with early AKI experienced shorter LOS than those with late AKI or both early and late AKI (early AKI: 90 ± 33 days vs. late AKI: 134 ± 49 days vs. both AKI: 124 ± 40 days). Similarly, in multivariable analysis, early AKI was associated with significantly shorter LOS while late AKI and both early and late AKI were associated with significantly longer LOS (Table 2).
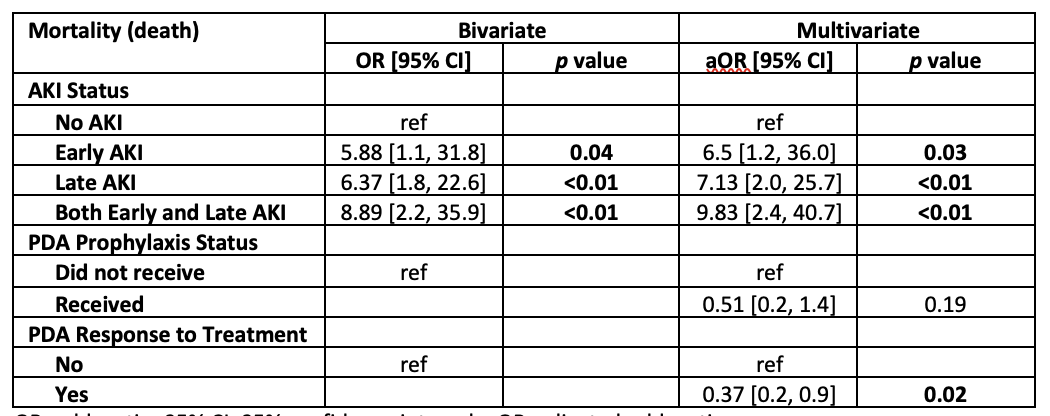
Mortality differed between AKI groups and was higher in those with any kind of AKI compared to those without AKI. In multivariate analysis, early AKI, late AKI and having both early and late AKI were strongly associated with increased odds of mortality (Table 3).
Conclusion(s):
In our single center cohort of ELBW infants with PDA, LOS and mortality did differ between neonates based on timing of AKI development. Notably, PDA ppx receipt and PDA status relative to treatment significantly impacted associations between AKI groups and LOS and mortality.