Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
268 - The relationship between hypochloremia and linear growth among infants diagnosed with severe bronchopulmonary dysplasia in a level IV referral NICU.
Publication Number: 268.34

Rachel Russell, MS (she/her/hers)
Medical Student
University of Arizona College of Medicine - Phoenix
Phoenix, Arizona, United States
Presenting Author(s)
Background:
Bronchopulmonary dysplasia (BPD) is a chronic lung disease in preterm infants following exposure to positive pressure respiratory support. Pulmonary edema is a complication of BPD that may result in impaired lung function, for which diuretics are often used. Hypochloremia, a common side effect of diuretics, is known to have an inverse relationship with growth in infants and, in a small study in infants with BPD, was associated with increased mortality. Linear growth is directly correlated with better clinical outcomes in infants with BPD. To date, the relationship between hypochloremia and linear growth has not been systematically evaluated in the BPD population.
Objective:
The purpose of this study is to determine the relationship between hypochloremia and linear growth among infants with severe BPD (sBPD) in a single center referral population.
Design/Methods:
A retrospective chart review was conducted for infants < 32 weeks birth gestational age (GA) with sBPD admitted to Phoenix Children’s NICU between January 2015 and March 2022. Frequency of hypochloremia (plasma chloride < 96mMol/L) was defined as number of weeks during NICU hospitalization with ≥1 instance of hypochloremia per total weeks in the NICU. Demographic and in-hospital outcome variables were compared using t-tests, Fisher’s exact tests, and chi squared tests. A Pearson correlation was performed between frequency of hypochloremia and change in length z-score between admission and discharge or death and length of stay (LOS).
Results:
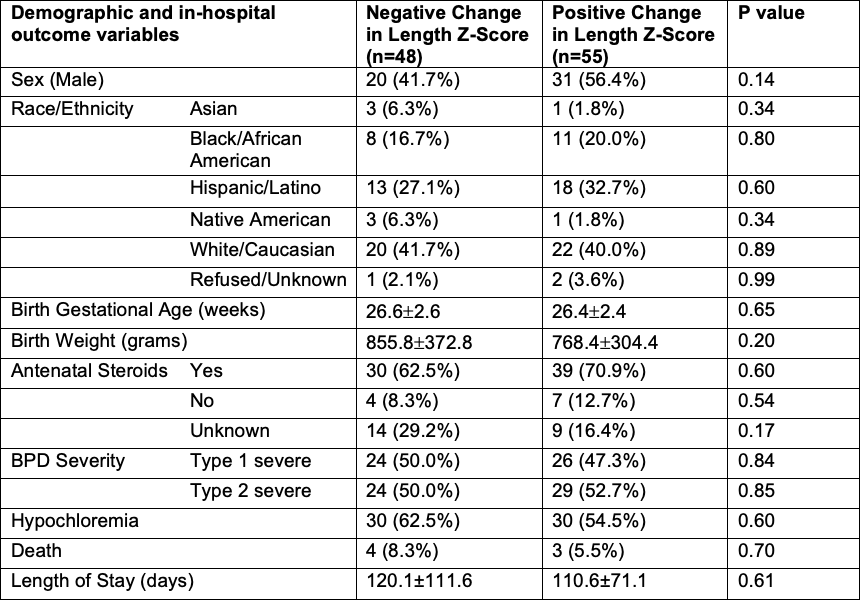
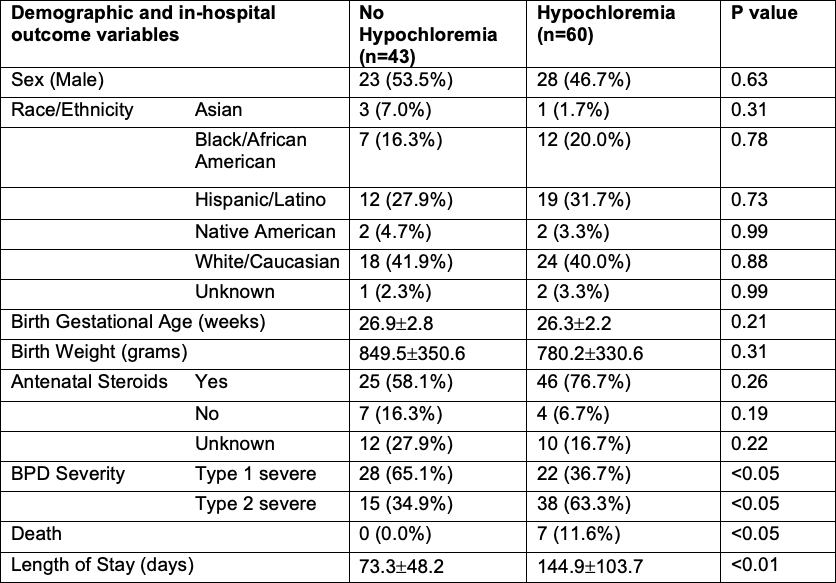
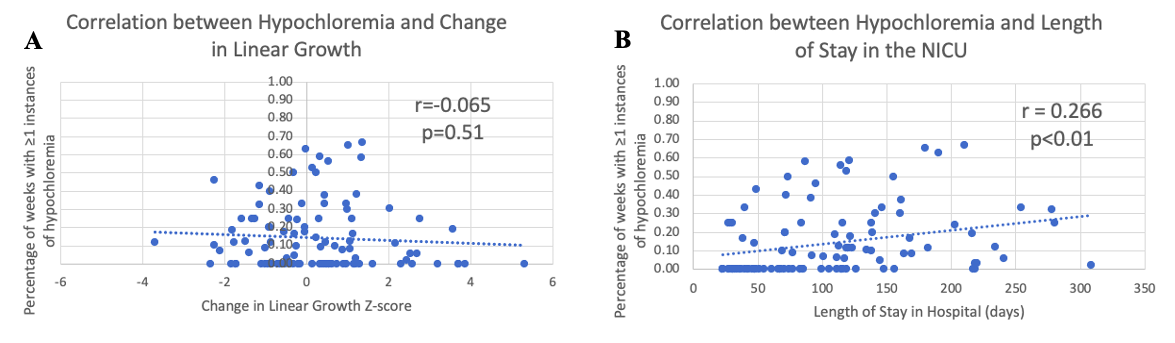
A total of 103 infants were included with an average GA of 26.5 weeks and birth weight of 809 grams. Forty-nine percent were male and survival was 93%. Hypochloremia occurred in 58% and positive linear growth in 53%. Demographic and outcome variables between infants who had a negative or positive change in length z score are similar (Table 1). When stratified by presence of hypochloremia, there is a greater frequency of type 2 sBPD (63% vs 35%, p< 0.05), death (11.7% vs 0%, p< 0.05), and longer LOS (145±104 days vs 73±48 days, p< 0.01) for those with hypochloremia (Table 2). There is no correlation between frequency of hypochloremia and change in linear growth (p=NS) but there is a positive correlation between frequency of hypochloremia and LOS (r=0.26, p< 0.01) (Figure 1).
Conclusion(s):
No correlation between hypochloremia and linear growth was demonstrated in this analysis. A positive correlation between hypochloremia and LOS was shown, suggesting hypochloremia is a marker of illness severity in sBPD. Additional investigation of thresholds and related variables is needed to further define relationships.