Neonatal Quality Improvement
Neonatal Quality Improvement 4
735 - Sixty Golden Minutes: A Golden Hour Bundle for High-Risk Preterm Infants
Publication Number: 735.343

Justin Kotliar, MD
Neonatal Fellow
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: The “Golden Hour” (GH) refers to the first sixty minutes after birth in neonates. In preterm infants, practice of evidence-based interventions during this GH has been associated with reduction in infant mortality and morbidities, including hypothermia, hypoglycemia, intraventricular hemorrhage, and bronchopulmonary dysplasia.
Objective: The primary aim was to increase overall adherence to the elements of the GH bundle to 50% by July 2023. Secondary aims were to: 1) reduce the rates of severe hypothermia (temperature < 36°C) by 25%, 2) reduce time to antibiotic administration by 25% and 3) increase the initiation of intravenous fluid (IVF) within the GH by 25% by July 2023.
Design/Methods:
A multidisciplinary quality improvement (QI) team performed sequential interventions in inborn newborns < 32 weeks or ≤1500 grams in a level IV NICU to reduce severe hypothermia, time to antibiotics and IVF administration (outcome measures). Our process measure was adherence to the GH standardized bundle. Baseline data was collected from January 2020 to July 2022. Balance measures included hyperthermia and admission temperature in preterm newborns that did not meet the GH inclusion criteria. Statistical process control charts and established Associates in Process Improvement rules for special cause variation were used to display and analyze data.
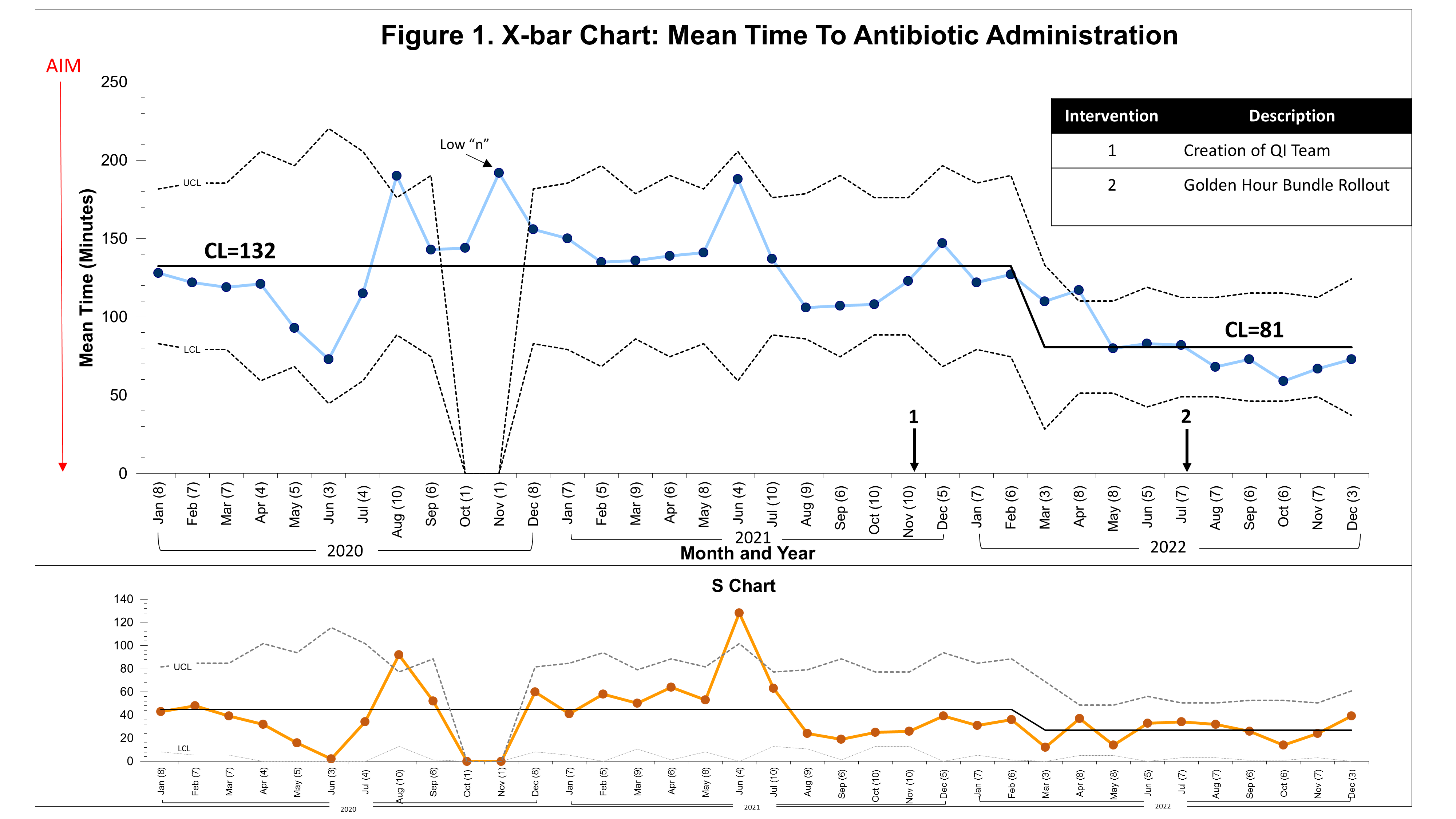
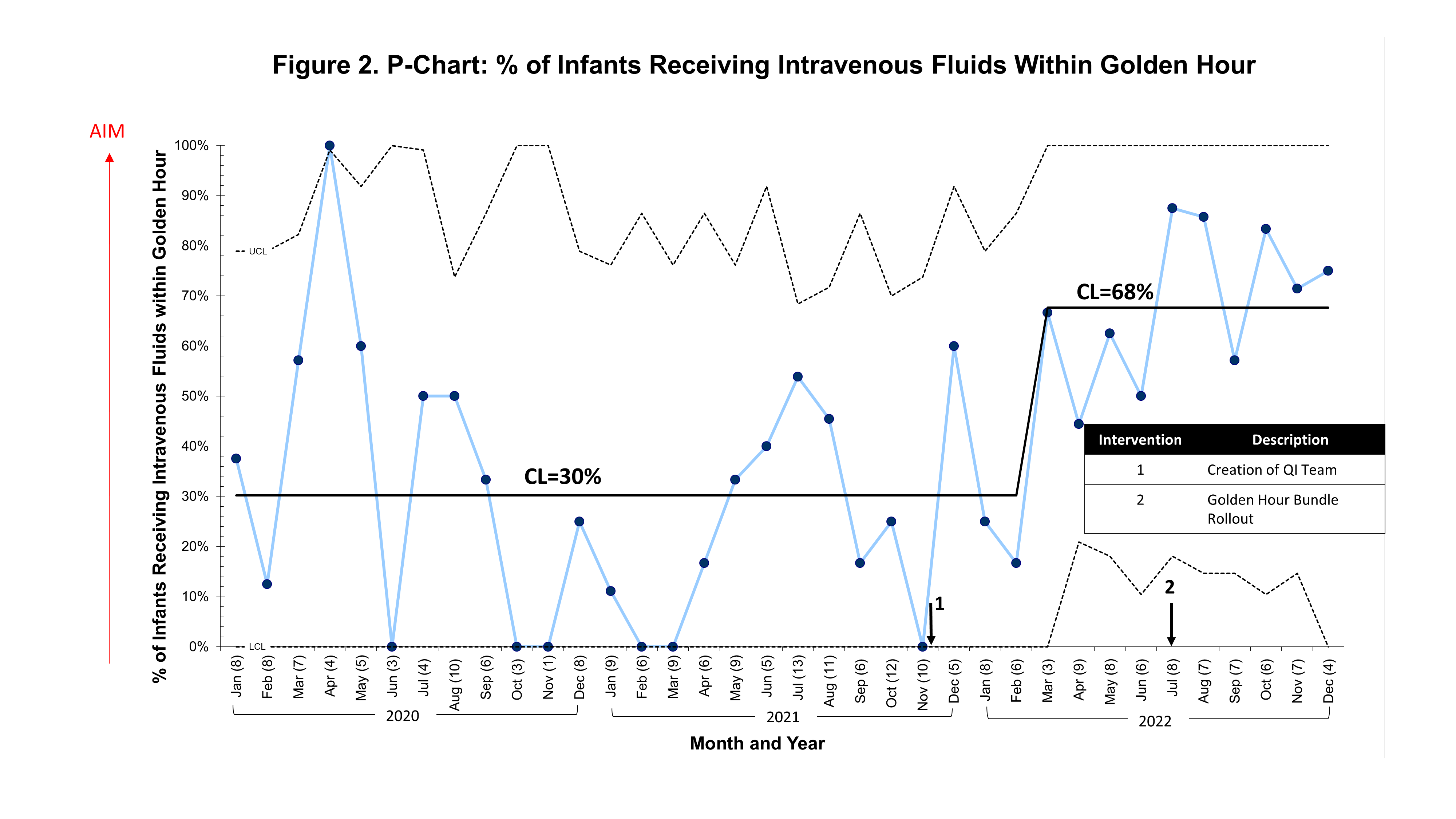
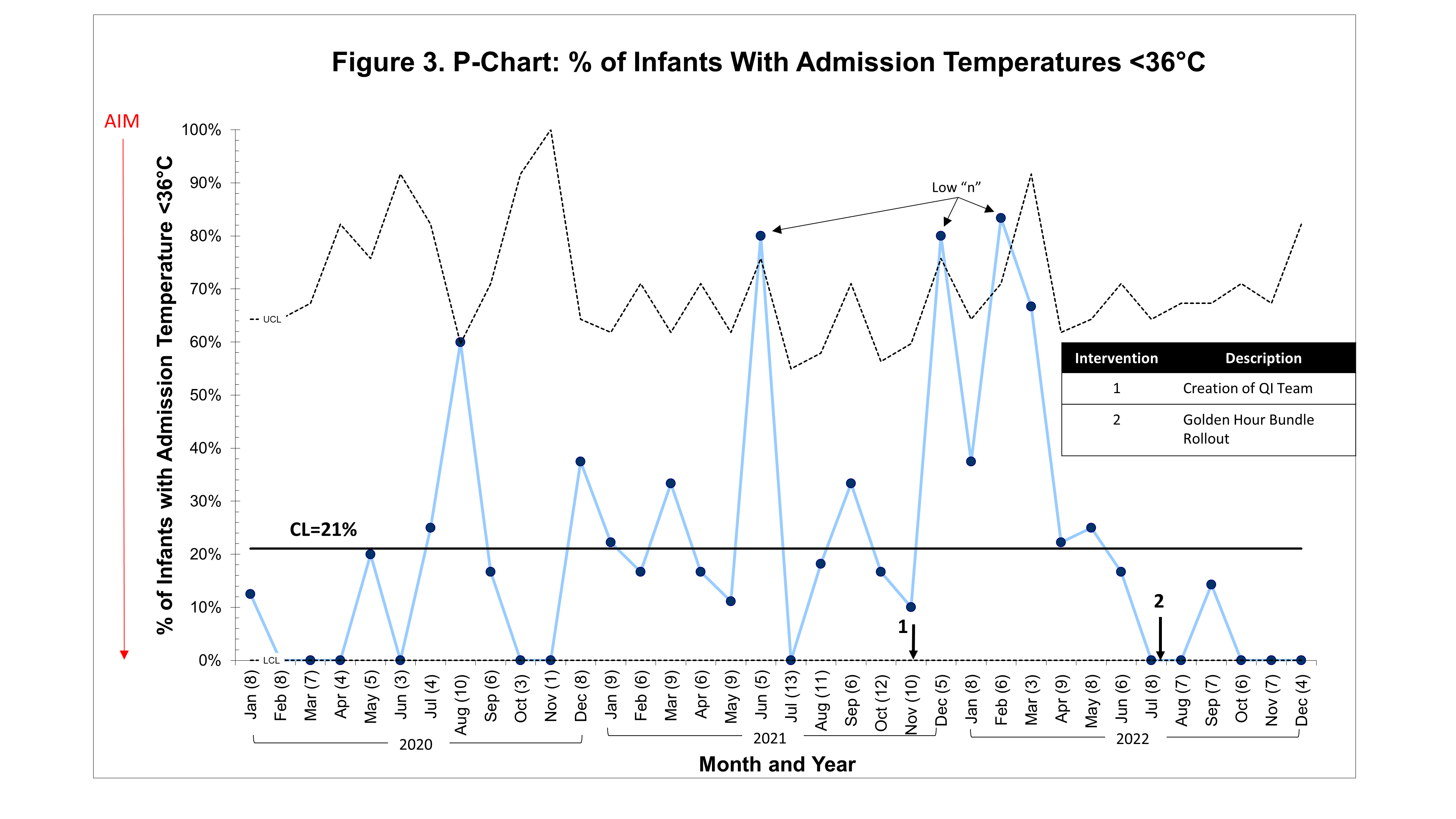
Results: A total of 247 infants were included (211 pre-GH bundle, 36 post-GH bundle). Mean gestational age and birth weight pre/post-GH bundle were 29 4/7 weeks, 1202 grams and 29 weeks, 1179 grams respectively. The adherence to the GH bundle was 89%. In regards to outcome measures, the mean time to antibiotic administration decreased from 132 minutes to 81 minutes (Figure 1) and the percentage of infants receiving IVF within the GH increased from 30% to 68% (Figure 2). The center line (CL) remained at 21% for severe hypothermia (Figure 3); however, we anticipate a CL change given the recent trend of seven consecutive points below the CL. For balance measures, there were no cases of hyperthermia or increased rates of hypothermia in excluded preterm newborns.
Conclusion(s): A multidisciplinary QI team successfully and safely demonstrated adherence to the GH bundle and subsequently an improvement in time to antibiotic administration and IVF initiation. While not yet special cause variation, initial efforts illustrate a trend towards reducing severe hypothermia. Future plans include incorporating the GH interventions as part of a larger bronchopulmonary dysplasia prevention bundle QI initiative.