Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
341 - Observational study comparing heart rate in crying and non-crying but breathing infants at birth
Publication Number: 341.346

Sara Berkelhamer, MD (she/her/hers)
Associate Professor or Pediatrics
University of Washington School of Medicine
Seattle, Washington, United States
Ashish KC, State University (he/him/his)
Associate Professor
Uppsala University
Uppsala, Uppsala Lan, Sweden
Presenting Author(s)
Co-Author(s)
Background:
Stimulation of breathing infants to elicit a cry is a common practice in newborn deliveries. However, international resuscitation algorithms disagree on whether crying or breathing should guide providing stimulation.
Objective:
Evaluate heart rate in infants who were crying versus non-crying but breathing immediately after birth.
Design/Methods:
This was single-center observational study of singleton vaginally born infants at ≥33 weeks of gestation in Nepal. Infants who were crying or non-crying but breathing within 30 seconds after birth were included. Background demographic data and delivery room events were recorded using tablet-based applications and synchronized with continuous heart rate data recorded by a dry-electrode electrocardiographic monitor. Heart rate centile curves were generated with piece wise regression analysis. Odds of bradycardia (heart rate < 100 bpm) and tachycardia (heart rate ≥200 bpm) during the first 180 seconds after birth were compared using logistic regression.
Results:
1155 crying and 54 non-crying but breathing infants were included. There were no significant differences in the demographic and obstetric factors between the cohorts (Table 1). Non-crying but breathing infants had higher rates of early cord clamping < 60s after birth (75.9% vs 46.5%) and admission to the neonatal intensive care unit (13.0% vs 4.3%), (Table 1-2). Non-crying but breathing infants had higher odds of bradycardia (adjusted odds ratio 2.64; 95% CI, 1.34-5.17) and tachycardia (aOR, 2.86; 95% CI, 1.50-5.47) (Table 3). Bradycardia appeared early whereas tachycardia was a relatively late phenomenon in non-crying but breathing infants (Figure 2a-b).
Conclusion(s): Non-crying but breathing infants have increased risk of bradycardia, tachycardia and neonatal intensive care admission compared to crying infants. This finding supports that non-crying but breathing infants be closely observed for clinical deterioration. This finding supports that non-crying but breathing infants should not be on the same care pathway as crying, and that close observation of these infants with risk for clinical deterioration is indicated.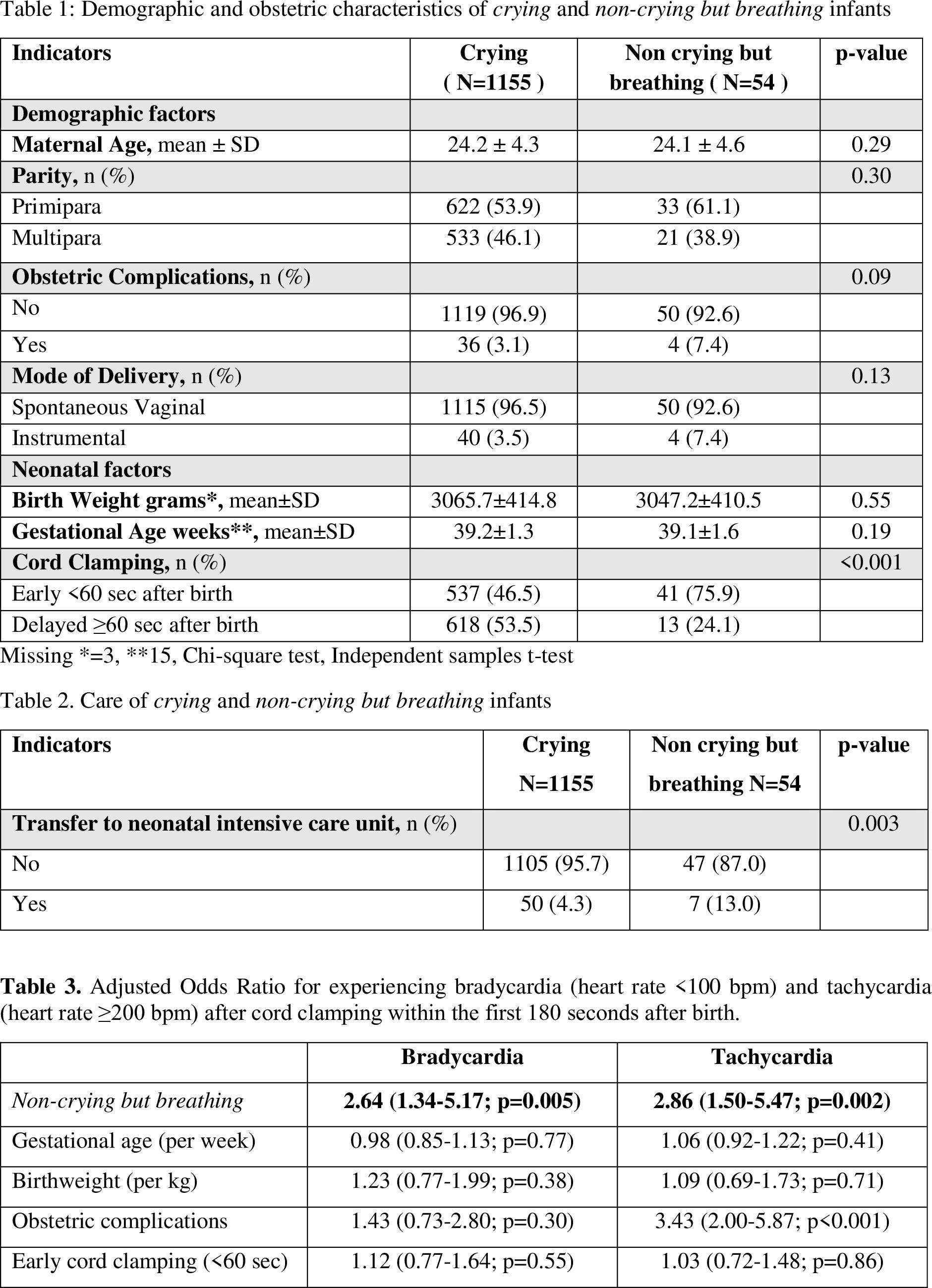
.jpg)
.png)
