Emergency Medicine: Quality Improvement
Emergency Medicine 10
466 - Introduction of Central Catheter Associated Bloodstream Infections Clinical Pathway in the Pediatric Emergency Department
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 466
Publication Number: 466.309
Publication Number: 466.309
Monica Saladik, OHSU, Portland, OR, United States; Mikelle Bassett, Doernbecher Children's Hospital at Oregon Health & Science University, portland, OR, United States; Beech S. Burns, Oregon Health & Science University, Portland, OR USA, OR, United States; Michelle Noelck, Oregon Health & Science University School of Medicine, Portland, OR, United States

Monica Saladik, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
OHSU
Portland, Oregon, United States
Presenting Author(s)
Background: Indwelling central venous catheters (CVC) carry risk of complications including central catheter-associated bloodstream infections (CCABSIs). To address the significant CCABSI risk we developed a standardized clinical pathway for patients with CVCs who present with concern for infection and implemented a quality improvement project to promote its use.
Objective: Standardize the emergency department (ED) management of non-oncology pediatric patients with a CVC who present with signs of infection, with the goals of increasing blood culture rates, empiric antibiotics use, and admission rates compared to baseline data.
Design/Methods: A clinical pathway was created by a multi-disciplinary team of providers by reviewing current literature, expert consensus, and review of local antibiograms. Baseline data was obtained for a 2-year time period between June 1st 2019-June 30th 2021. After pathway implementation we collected data on the process measure of order set usage; the outcome measures of blood culture rate, antibiotic initiation rate, bacteremia detection following discharge home, and hospital readmission rates; and balancing measures of average hospital admission days and number of patients admitted to the hospital who ultimately have negative blood cultures.
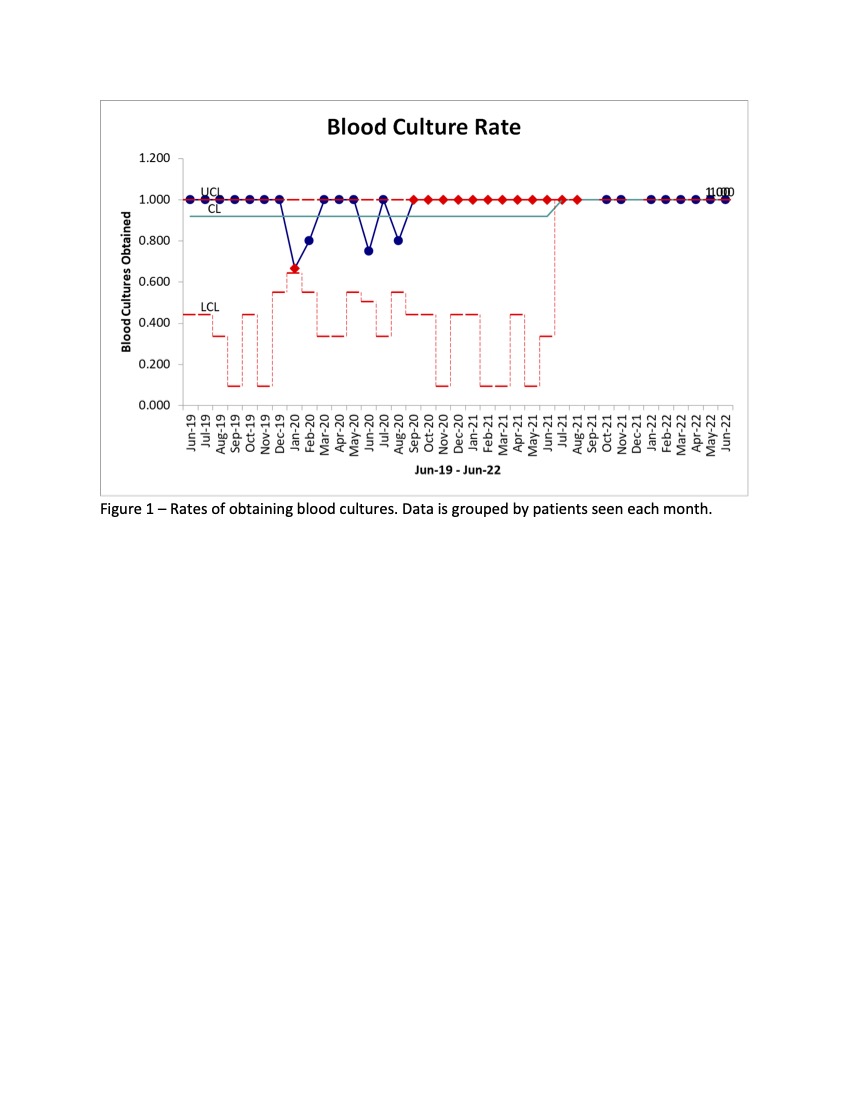
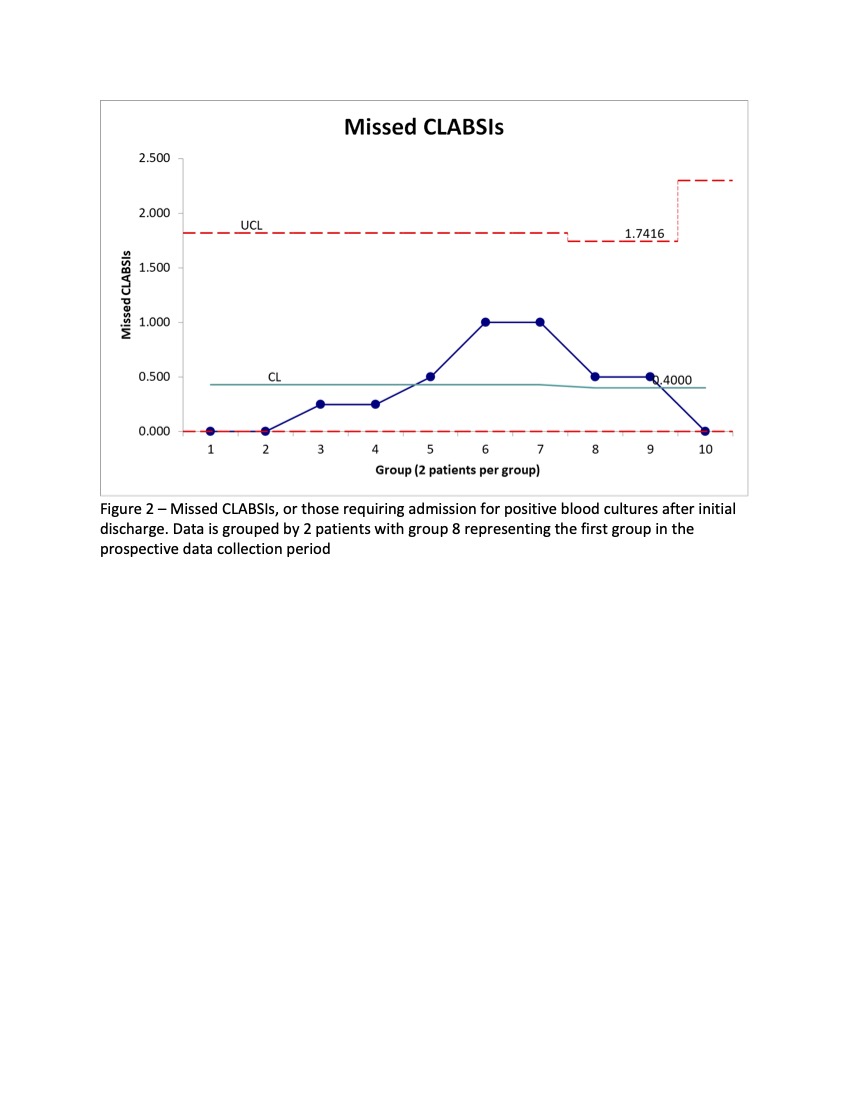
Results: A total of 73 patients met inclusion criteria in the baseline period compared to 23 patients in the first year of prospective data collection. Table 1 outlines patient characteristics and outcomes pre-and post-intervention. Order set usage in the post-intervention period was 30%. Rates of obtaining blood cultures improved after pathway implementation (Figure 1), from 92% to 100%, as did rate of antibiotic initiation, from 74% to 83%, though the difference was not statistically significant. Comparing the pre- and post-implementation periods, there was no significant difference in the p</span>roportion of patients discharged who had true bacteremia requiring readmission after ED discharge (21% vs 20%) (Figure 2) and no difference in average admission days.
Conclusion(s): Through implementation of a clinical pathway, we trended toward improved rates of blood cultures acquisition, rates of antibiotic administration, and better identification of those requiring admission. Ongoing improvement efforts include focus on appropriate initial antibiotic choice and future potential for decreasing time to antibiotic administration.
.jpg)
