Back
Background: The concern for acute appendicitis accounts for a large percentage of pediatric emergency department (ED) visits each year. It is currently unknown what percentage of these referrals to an ED have a final diagnosis of appendicitis after evaluation. Unnecessary referrals for appendicitis may have implications on time, resources, and cost for patients, their families, the overwhelmed ED, and the health care system.
Objective: To analyze pediatric referrals for definitive or possible appendicitis, to compare clinical predictors and laboratory values between patients with and without a final diagnosis of appendicitis, and to determine the accuracy of pre-referral diagnostic interpretations of CT scans, ultrasound, and MRI modalities.
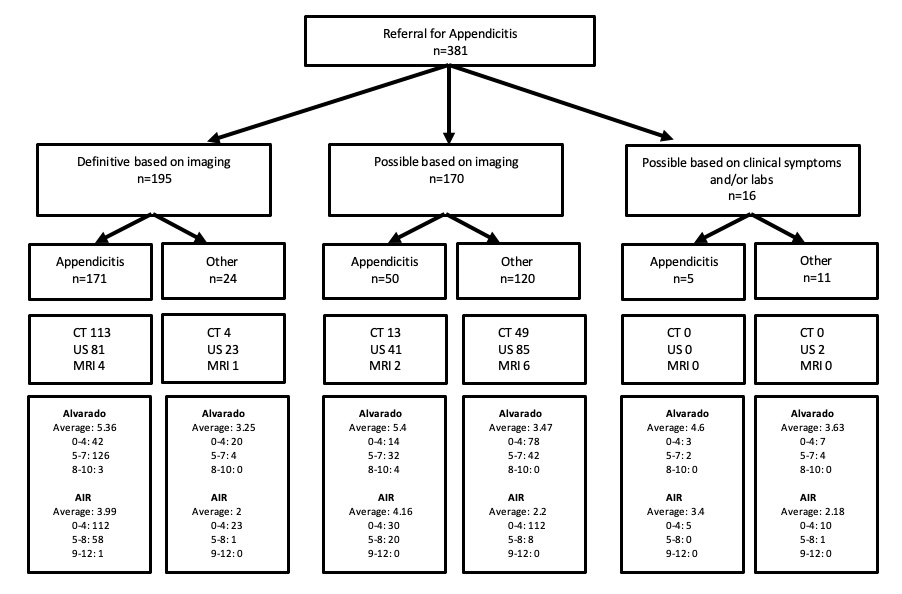
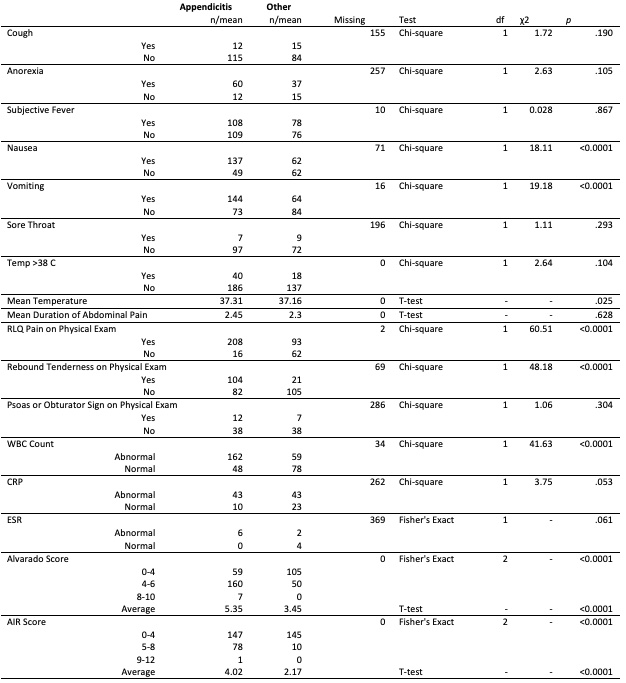
Design/Methods: We conducted a retrospective analysis of pediatric patients referred from 2015-2019 to a tertiary care children’s ED with definitive or possible appendicitis. Data abstracted included patient demographics, clinical symptoms, physical exam findings, laboratory results, and diagnostic imaging findings (by the referring center and the pediatric radiologist at the accepting center). An Alvarado and Appendicitis Inflammatory Response (AIR) score was calculated for each patient.
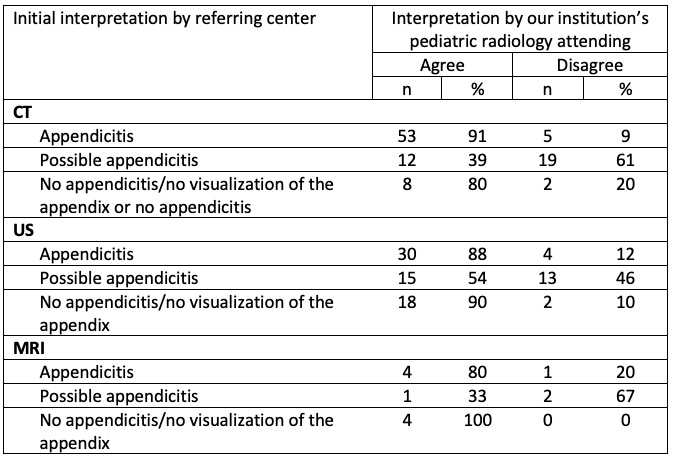
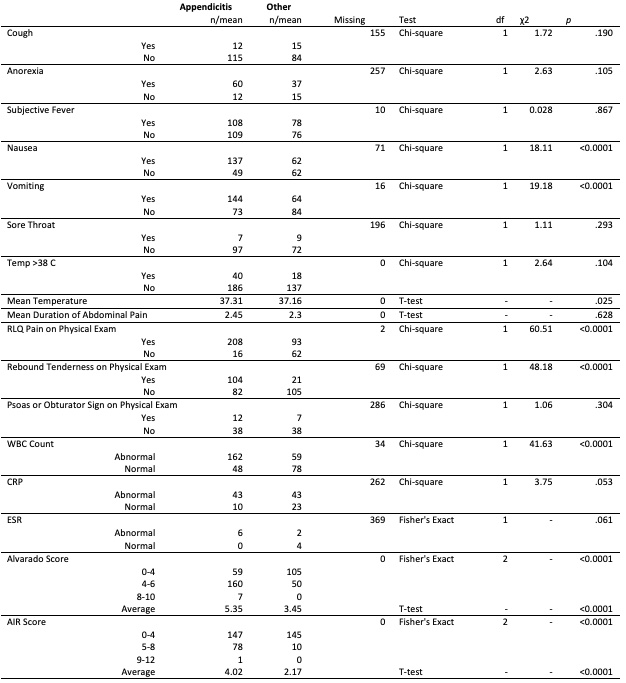
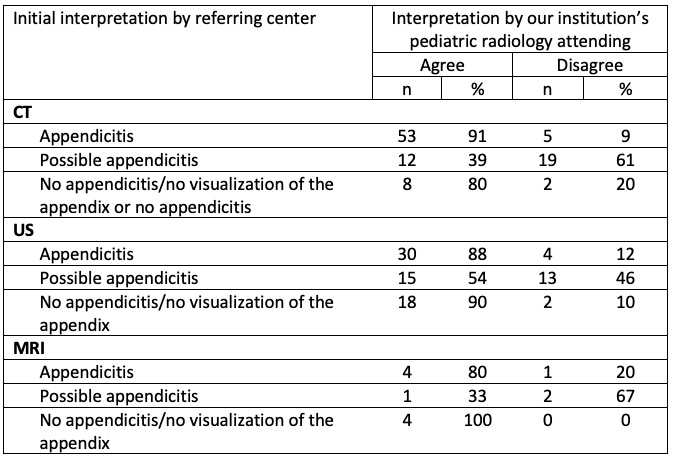
Results: Analysis was performed on 381 patients; 226 (59%) had a final diagnosis of appendicitis. Patients with appendicitis were more likely to have symptoms of nausea (p< 0.0001) and vomiting (p< 0.0001), have a higher mean temperature (p=0.025), right lower quadrant abdominal pain to palpation (p=< 0.0001), rebound tenderness (p< 0.0001), a higher mean Alvarado score [5.35 vs. 3.45 (p< 0.0001)], and a higher mean AIR score [4.02 vs. 2.17 (p< 0.0001)]. Of the 97 diagnostic images initially interpreted as appendicitis by the referring center, 10 (10.3%) were read as no evidence of appendicitis. Of the 62 diagnostic images initially interpreted as "possible appendicitis" by the referring center, 34 (54.8%) were read as no evidence of appendicitis. Of those diagnostic images initially interpreted as "appendicitis" or "possible appendicitis" by the referring center, 24/89 (27.0%) of CT scans, 17/62 (27.4%) of USs, and 3/8 (37.5%) of MRIs were read as no evidence of appendicitis.
Conclusion(s): Utilization of established scoring algorithms, such as Alvarado and AIR, may decrease the unnecessary cost of diagnostic imaging and transfer to tertiary care. Virtual radiology consultations may be one potential solution to improve the referral process for pediatric appendicitis if initial interpretation is uncertain.
Emergency Medicine: All Areas
Emergency Medicine 12
499 - Referrals for Pediatric Appendicitis to a Tertiary Care Children’s Hospital
Sunday, April 30, 2023
3:30 PM – 6:00 PM ET
Poster Number: 499
Publication Number: 499.311
Publication Number: 499.311
Elise McNulty, Penn State College of Medicine, Hershey, PA, United States; Robert P. Olympia, Penn State University, Hershey, PA, United States; Alicia C. Greene, Penn State Hershey Medical Center, Hershey, PA, United States; Anthony Tsai, Penn State Children's Hospital, Hershey, PA, United States

Elise McNulty, MHS (she/her/hers)
Medical Student
Penn State College of Medicine, Pennsylvania, United States
Presenting Author(s)
Background: The concern for acute appendicitis accounts for a large percentage of pediatric emergency department (ED) visits each year. It is currently unknown what percentage of these referrals to an ED have a final diagnosis of appendicitis after evaluation. Unnecessary referrals for appendicitis may have implications on time, resources, and cost for patients, their families, the overwhelmed ED, and the health care system.
Objective: To analyze pediatric referrals for definitive or possible appendicitis, to compare clinical predictors and laboratory values between patients with and without a final diagnosis of appendicitis, and to determine the accuracy of pre-referral diagnostic interpretations of CT scans, ultrasound, and MRI modalities.
Design/Methods: We conducted a retrospective analysis of pediatric patients referred from 2015-2019 to a tertiary care children’s ED with definitive or possible appendicitis. Data abstracted included patient demographics, clinical symptoms, physical exam findings, laboratory results, and diagnostic imaging findings (by the referring center and the pediatric radiologist at the accepting center). An Alvarado and Appendicitis Inflammatory Response (AIR) score was calculated for each patient.
Results: Analysis was performed on 381 patients; 226 (59%) had a final diagnosis of appendicitis. Patients with appendicitis were more likely to have symptoms of nausea (p< 0.0001) and vomiting (p< 0.0001), have a higher mean temperature (p=0.025), right lower quadrant abdominal pain to palpation (p=< 0.0001), rebound tenderness (p< 0.0001), a higher mean Alvarado score [5.35 vs. 3.45 (p< 0.0001)], and a higher mean AIR score [4.02 vs. 2.17 (p< 0.0001)]. Of the 97 diagnostic images initially interpreted as appendicitis by the referring center, 10 (10.3%) were read as no evidence of appendicitis. Of the 62 diagnostic images initially interpreted as "possible appendicitis" by the referring center, 34 (54.8%) were read as no evidence of appendicitis. Of those diagnostic images initially interpreted as "appendicitis" or "possible appendicitis" by the referring center, 24/89 (27.0%) of CT scans, 17/62 (27.4%) of USs, and 3/8 (37.5%) of MRIs were read as no evidence of appendicitis.
Conclusion(s): Utilization of established scoring algorithms, such as Alvarado and AIR, may decrease the unnecessary cost of diagnostic imaging and transfer to tertiary care. Virtual radiology consultations may be one potential solution to improve the referral process for pediatric appendicitis if initial interpretation is uncertain.