Allergy, Immunology and Rheumatology
Allergy, Immunology, and Rheumatology
378 - Changes in Hospitalization Rates of Kawasaki Disease Before and During the COVID19 Pandemic: A Nationwide Population-Based Study
Publication Number: 378.301

Eyal Bendavid, MD (he/him/his)
Resident Physician
Harbor-UCLA Medical Center
Torrance, California, United States
Presenting Author(s)
Background:
A significant decrease in Kawasaki disease (KD) incidence rate during the COVID-19 pandemic has been reported globally. This decrease is likely due to infection prevention measures such as social distancing and the decreased circulation of other respiratory viruses with which KD has been reported to be associated.
Objective:
We aim to perform nationwide population-based analyses for patients with KD during the COVID-19 pandemic for the year 2020, evaluating the characteristics of this cohort with patients from the previous 4 years, using the largest nationwide inpatient database in the U.S.
Design/Methods:
We identified pediatric patients diagnosed with KD (KD patients) in the National (Nationwide) Inpatient Sample between 2016 and 2020.
Hospitalization rate, length of stay (LOS), and hospitalization cost per day (cost/day) among KD patients were evaluated. Stratified analyses by race/ethnicity, age groups, and geographical region were performed. Regression models adjusted by patient and hospital characteristics were used to evaluate the associations of the pandemic with LOS and cost/day.
Results:
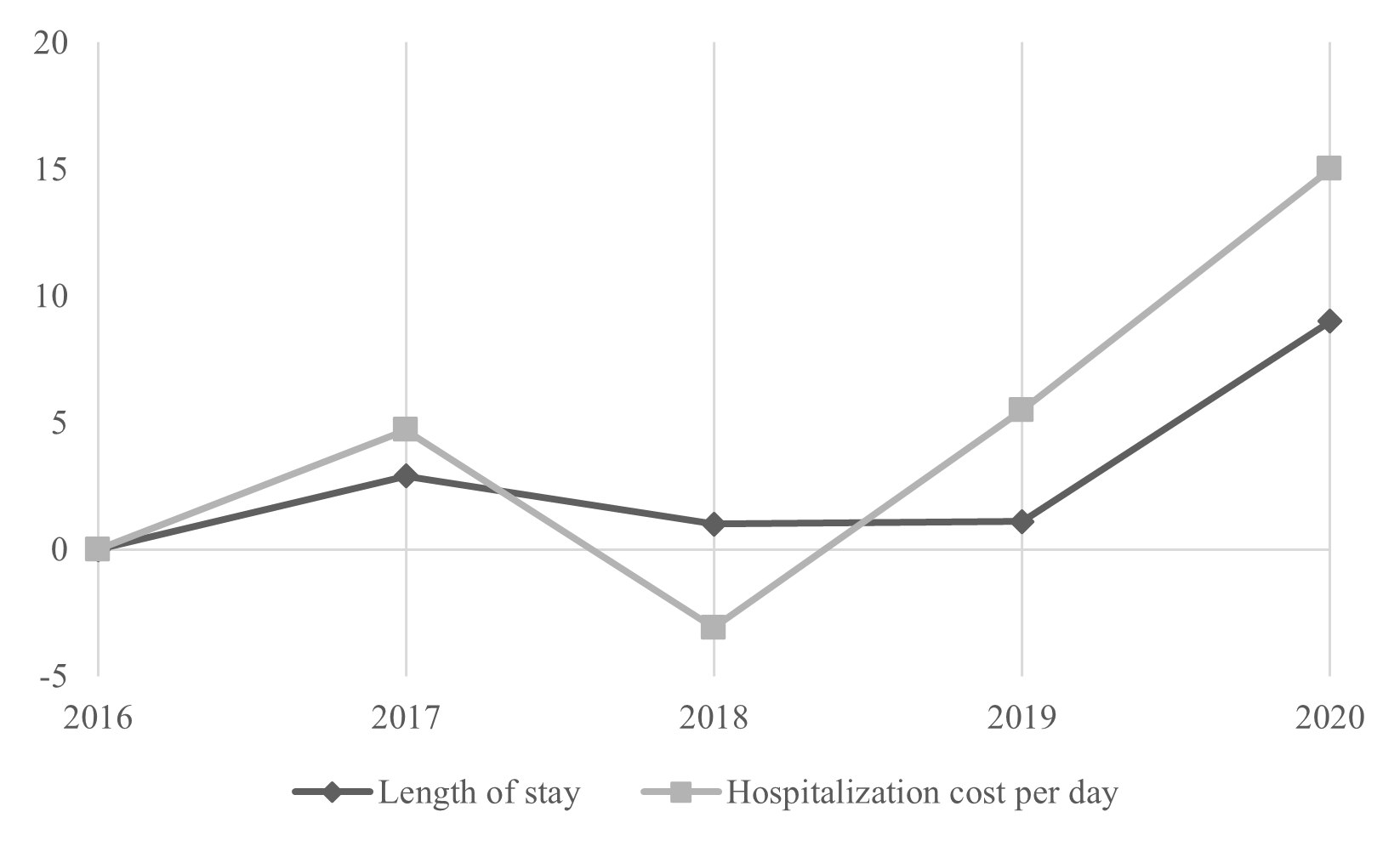
We identified 20,255 and 4,250 pediatric KD patients, yielding hospitalization rates of 65.1 and 53.8 per 1,000,000 during the pre-pandemic and pandemic periods, respectively. Hospitalization rates were reduced by the greatest percentage among patients between 1-4 years old (26.2%), male (19.1%), and Asian or Pacific Islander (33.2%). We also found a substantially smaller reduction in the hospitalization rate for KD in the Northeast (NE) (3.5%) compared to other regions. Associations of the pandemic with longer LOS and higher cost/day were detected (adjusted mean ratio [aMR] 1.11, p < .01 for LOS, and aMR 1.19, p < .01 for cost/day). Although LOS and cost/day already exhibited increasing trends before pandemic, the increases from the previous year were substantially larger in 2020 compared to other years. (< 3.0% vs 9.0% for LOS and < 5.0% vs 15.0% for cost/day)
Conclusion(s):
Impact of the pandemic and infection prevention measures differed across age, race/ethnicity, and regions. NE had a higher population density compared to other groups. Thus, residents in NE were more likely to be exposed to human-to-human contact leading to the exposure to unidentified agents which can trigger KD causing to a smaller decrease in KD hospitalization during the pandemic compared to other regions as shown in a higher number of COVID-19 cases per population. Substantially larger increases in LOS and cost/day in 2020 suggest that increased LOS and cost/day is associated with the pandemic instead of general increasing trends.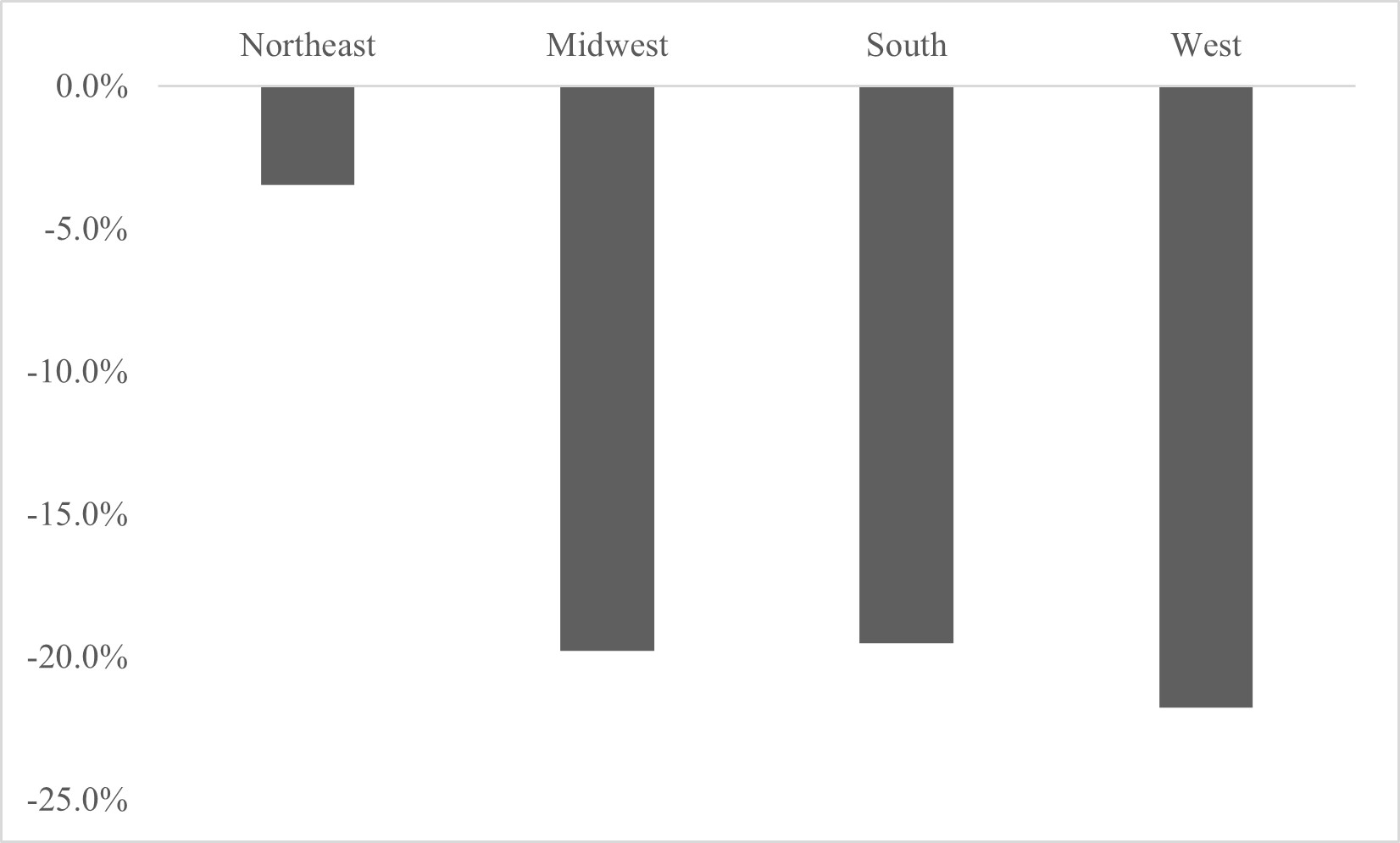
.jpg)
