Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 1
219 - National Trend of Use and Outcomes of Percutaneous Patent Ductus Arteriosus Closure in Newborn Infants
Publication Number: 219.329

Arpit Gupta, MD, FAAP (he/him/his)
Attending Physician
New York Medical College/Metroplitan Hospital Center
NYC, New York, United States
Presenting Author(s)
Background:
Percutaneous (catheter-based) closure is considered the procedure of choice in children > 6 kg with patent ductus arteriosus (PDA) with an increasing interest in newborns. However, data regarding the outcomes of percutaneous PDA closure in neonates are scarce.
Objective: To evaluate national trend of percutaneous PDA closure rates and outcomes in newborns.
Design/Methods:
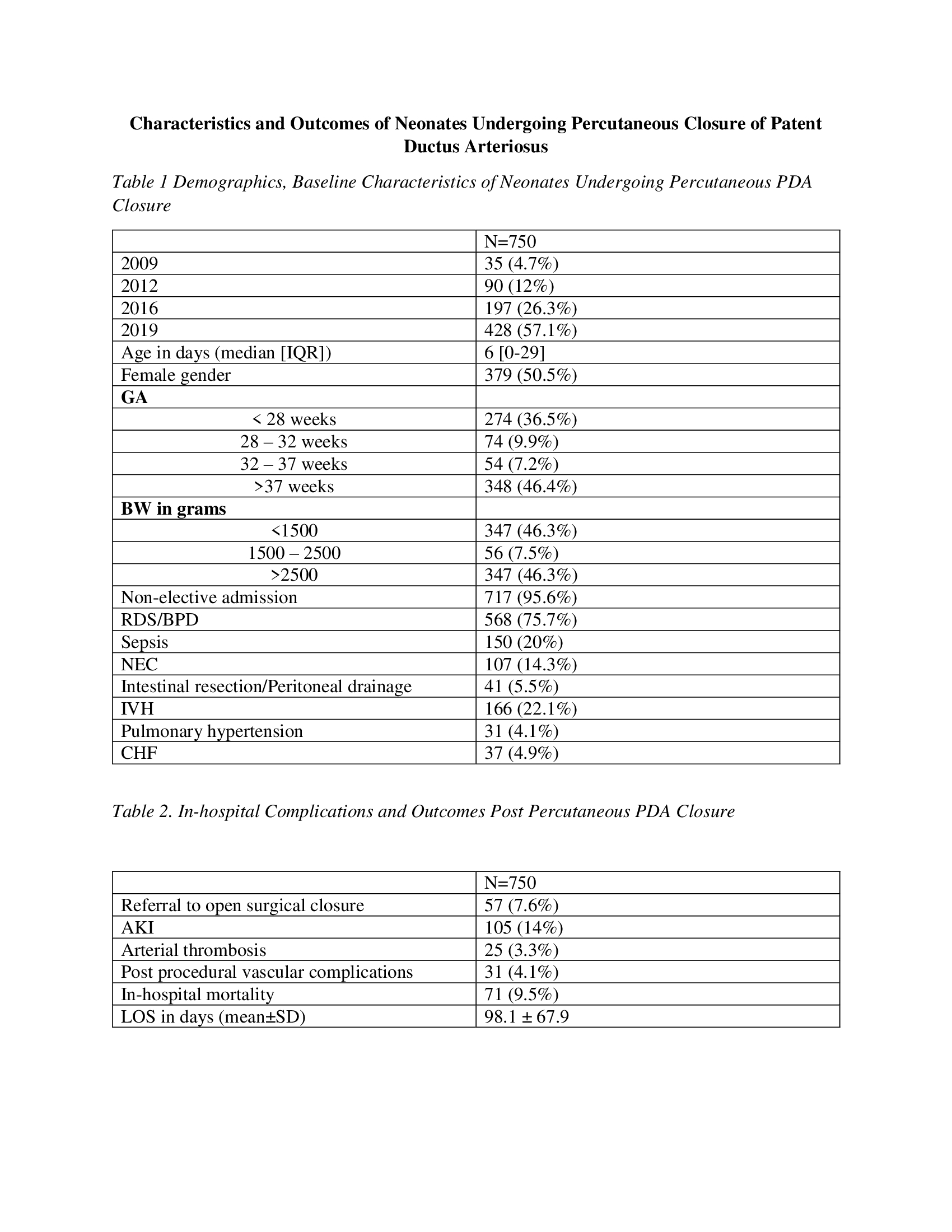
Hospitalizations of 166,583 neonates (≤28 days) with PDA were identified from the Kids’ Inpatient Database in 2009, 2012, 2016, and 2019. Of them, 750 patients underwent percutaneous PDA closure (mean age; 5.8 ± 7.6 days, and 50.5% females). Characteristics and outcomes were analyzed.
Results:
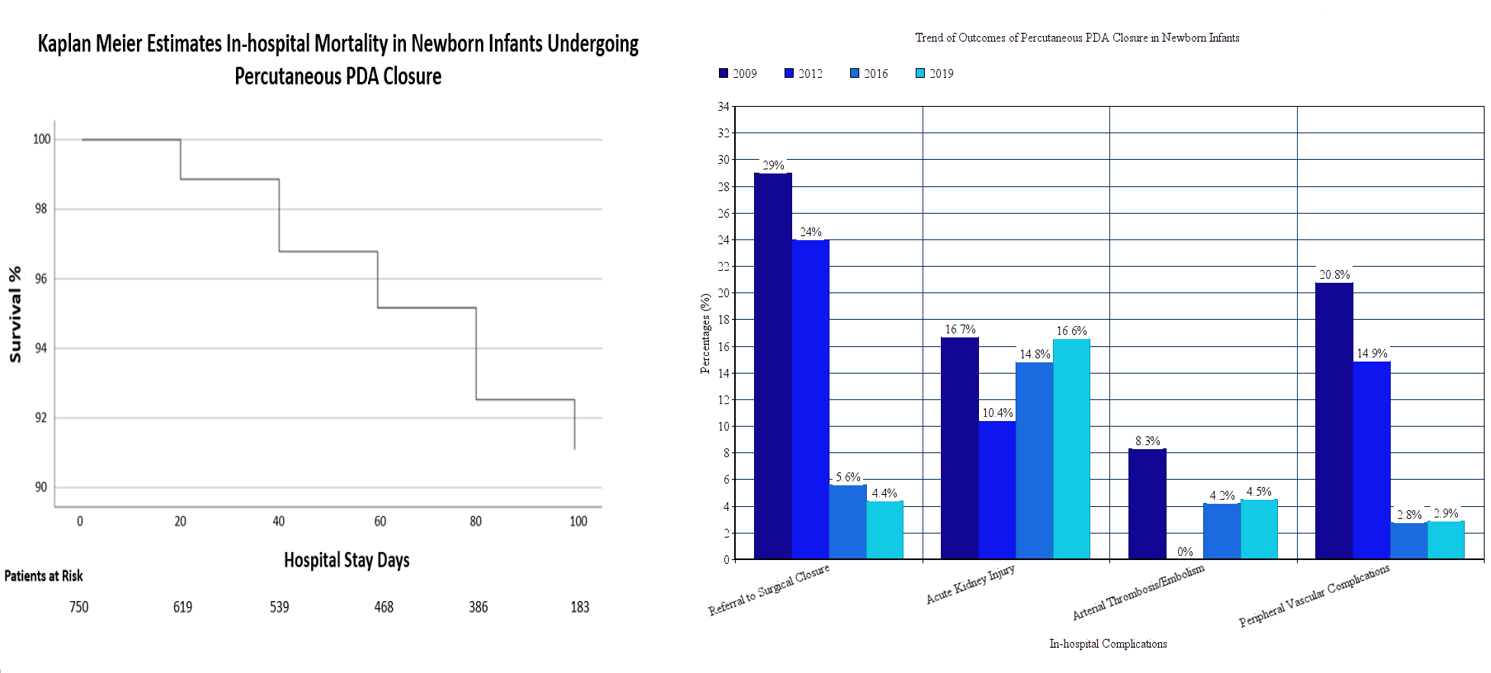
The incidence of percutaneous PDA closure has increased over the years (0.1% in 2009, and 0.9% in 2019). Birth weight (BW) was < 1500 g in 347 patients (46.3%), and gestational age was < 32 weeks in 348 patients (45.6%). Forty-one patients (5.5%) had necrotizing enterocolitis requiring surgery. Referral to surgical closure was required in 57 patients (7.6%), of them 5 patients (1.7%) were born < 1500 grams. Incidence of referral declined from 20% in 2009 to 4.4% in 2019. Procedural complications included acute kidney injury in 14%, arterial thrombosis in 3.3%, and peripheral vascular complications in 4.1%. Overall in-hospital mortality was 9.5%. Younger age during procedure, and BW < 1500 g were predictors of in-hospital mortality.
Conclusion(s):
Percutaneous PDA closure is a reliable alternative to surgical ligation in neonates including those with very low birth weight. The success rate improved significantly across the years. Age at the time of procedure is inversely related to in-hospital mortality. These data can be considered in decision-making and family counseling.