Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 4: Surfactant and NIV 1
660 - CPAP Or Nasal Cannula Oxygen for Preterm Infants (COCO): A Randomized Clinical Trial
Publication Number: 660.442

Zaki Yazdi, MD
Neonatology Fellow
University of Alabama School of Medicine
Hoover, Alabama, United States
Presenting Author(s)
Background:
Continuous positive airway pressure (CPAP) and low flow nasal cannula (≤1 L/kg/min, NC) are common methods of respiratory support in preterm infants with resolving respiratory distress syndrome or evolving bronchopulmonary dysplasia.
Objective:
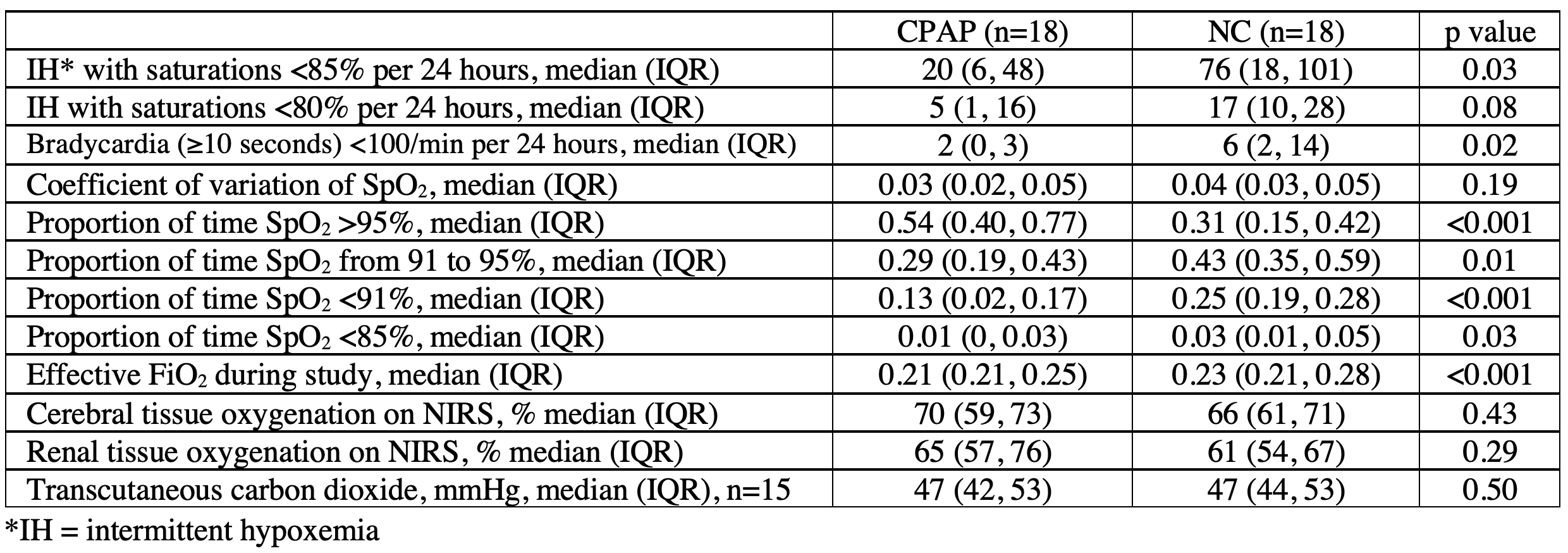
To determine if continuing CPAP compared with weaning to NC reduces intermittent hypoxemia (IH; defined as oxygen saturations (SpO2) < 85% for ≥10 seconds). Secondary outcomes included: the coefficient of variability of SpO2, the proportion of time with SpO2 in prespecified ranges ( > 95%, 91-95%, < 91%, < 85%), the number of episodes (≥ 10 seconds) with SpO2 less than 80%, median cerebral and renal oxygenation, median effective FiO2, median transcutaneous carbon dioxide, and episodes (≥ 10 seconds) of bradycardia < 100/min during each intervention.
Design/Methods:
Single center randomized clinical trial with a 1:1 parallel allocation of infants to CPAP or NC (0.5 L/kg/min up to a limit of 1.0 L/min). Preterm infants (gestational age < 34 weeks) receiving CPAP with a PEEP ≤5 and FiO2 ≤0.30 were eligible if meeting additional respiratory stability criteria. During a 24-hour intervention period, continuous cardiorespiratory data were collected from patient monitors. We required 38 infants (19 per group) to determine if continuing CPAP decreased IH from 130 to 85 episodes per 24 hours with a power of 90%, a two-tailed α of 0.05, and a standard deviation of 30 episodes, anticipating 20% crossover from NC to CPAP and 0% crossover from CPAP to NC. Results were analyzed with the Mann-Whitney U test.
Results:
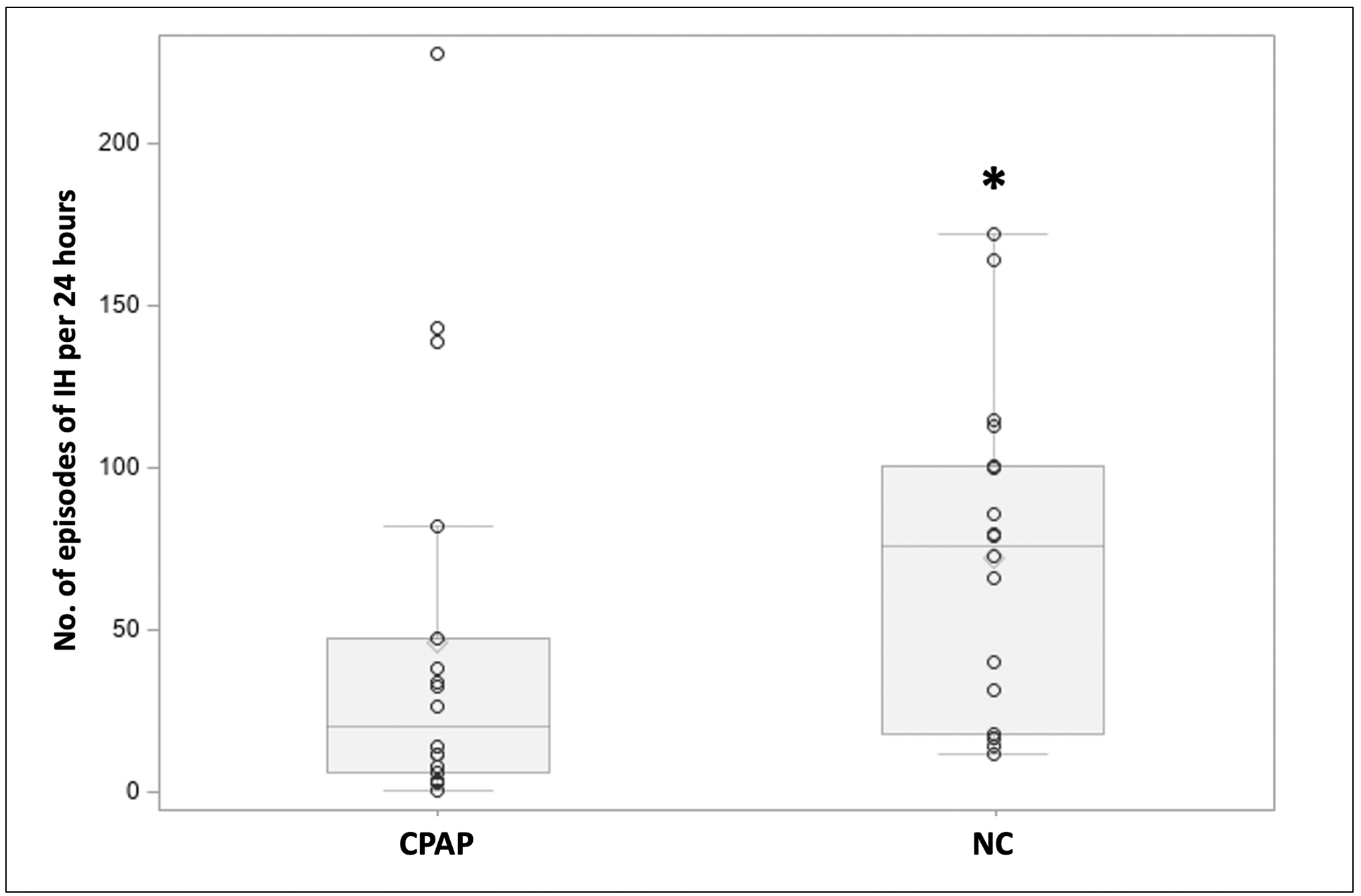
Thirty-eight infants were randomized, of whom two were excluded from analyses due to pre-specified criteria. The (mean ± SD) gestational age was 27 0/7 ± 2 weeks, birth weight was 933 ± 338 grams, and infants were studied at postnatal day 26 ± 29. The median (IQR) episodes of IH per 24-hour period was 20 (6, 48) in the CPAP group and 76 (18, 101) in the NC group (p=0.03) (Figure, Table). Infants continued on CPAP also had less bradycardia, time with SpO2< 91%, < 85%, 91-95%, and lower FiO2, as well as more time with SpO2>95% (Table). SpO2 stability did not differ (Table). There were no differences in IH < 80%, transcutaneous carbon dioxide, or cerebral/renal tissue oxygenation (Table).
Conclusion(s):
In preterm infants meeting respiratory stability criteria for CPAP cessation, continued CPAP decreased IH, bradycardia, and other measures of respiratory instability compared with weaning to NC. Ideal timing of CPAP cessation remains unclear, but continued CPAP may improve control of breathing.