Quality Improvement/Patient Safety: Subspecialty-specific QI: see specialties above
QI 4: Inpatient QI/Patient Safety
231 - Quality Improvement Project – Improving Accuracy of Blood Pressure Measurement in the Inpatient Children’s Hospital Setting
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 231
Publication Number: 231.45
Publication Number: 231.45
Alexis V. Hyczko, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Zeva Graf, Penn State Children's Hospital, Harrisburg, PA, United States; Michael A. Freeman, Penn State Children's Hospital, Hershey, PA, United States; Hannah Kim, Pennsylvania State University College of Medicine, Hershey, PA, United States

Zeva Graf, BS (she/her/hers)
Medical Student
Penn State Children's Hospital
Harrisburg, Pennsylvania, United States
Presenting Author(s)
Background: Measurement of blood pressure (BP) in the pediatric inpatient setting via AAP recommended methods can be challenging for many reasons including variability of patient age/size, intravenous lines in upper extremities, and supine positioning.
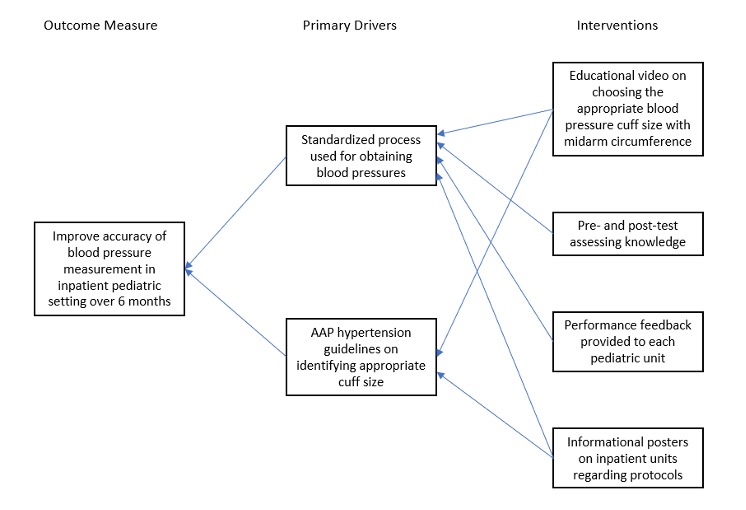
Objective: We aimed to improve appropriate BP cuff size usage.
Design/Methods: We conducted a single-center QI project with 2 cycles of Plan-Do-Study-Act on 2 floors within the PennState Children’s Hospital between July 2021 to July 2022. In the 1st cycle, we assessed a process measure defined as knowledge of appropriate BP cuff size via a pre- and post-test format with 3 hands-on cases and an educational video consistent with AAP hypertension guidelines. In the 2nd cycle, we assessed the outcome measure of appropriate BP cuff size choice in patient rooms before and after further education with posters in staff workspaces. Mann-Whitney rank sum and Chi-square analyses were used to assess factors associated with appropriate BP cuff size usage. We explored age, sex, BP cuff size, date of data collection, and patient location by floor.
Results: 55 and 35 subjects participated in the pre- and post-tests respectively. In the pre-test, 64% of participants answered 1 or more of 3 cases correctly. Post-test scores were noted to be worse than pre-test scores with only 11% of participants answering any of the cases correctly. The most common error was BP cuff size choice in younger subjects with obesity. 64% of patients were observed to have an appropriately sized BP cuff in their room prior to release of the educational posters with improvement to 75% following the intervention. In the 1st audit (n=47), there was no pattern noted between those who had a correctly sized BP cuff and those who did not when looking at patient age, sex, BP cuff size, nor floor the patient was on, but we did note a statistically significant pattern by day of data collection (p=0.039). In the 2nd audit (n=51) that pattern was no longer noted. We found that for those who had an inappropriate cuff size, the cuff size was more likely to be undersized than to be oversized.
Conclusion(s): There was an increase in appropriate BP cuff size usage for patients following education via multiple modalities including videos and posters which may be used for continued education. Test scores did not indicate similar improvement in BP measurement skills and may not be the best modality for assessment of knowledge. Day of data collection was significantly associated with appropriate BP cuff size use. We hypothesize that presence of/knowledge base of certain staff members may affect patient care.
.jpg)
