Quality Improvement/Patient Safety: Subspecialty-specific QI: see specialties above
QI 5: Quality Measures, Family Centered & Inpatient QI
243 - Implementation of a Serial Ultrasound Clinical Pathway to Reduce Ionizing Radiation Exposure in Patients with Suspected Appendicitis: A Quality Improvement Initiative
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 243
Publication Number: 243.451
Publication Number: 243.451
Zebulon Timmons, Children's Hospital & Medical Center, Omaha, Omaha, NE, United States; Tamara Pottker, Phoenix Children's Hospital, Scottsdale, AZ, United States; Craig Vander Wyst, Children's Hospital Colorado, Denver, CO, United States; Justin Lee, Phoenix Children's Hospital, Phoenix, AZ, United States; Blake Bulloch, Phoenix Children's Hospital, Phoenix, AZ, United States; Cecilia Monteilh, Phoenix Children's Hospital, Phoenix, AZ, United States

Cecilia Monteilh, MD
Attending Physician
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
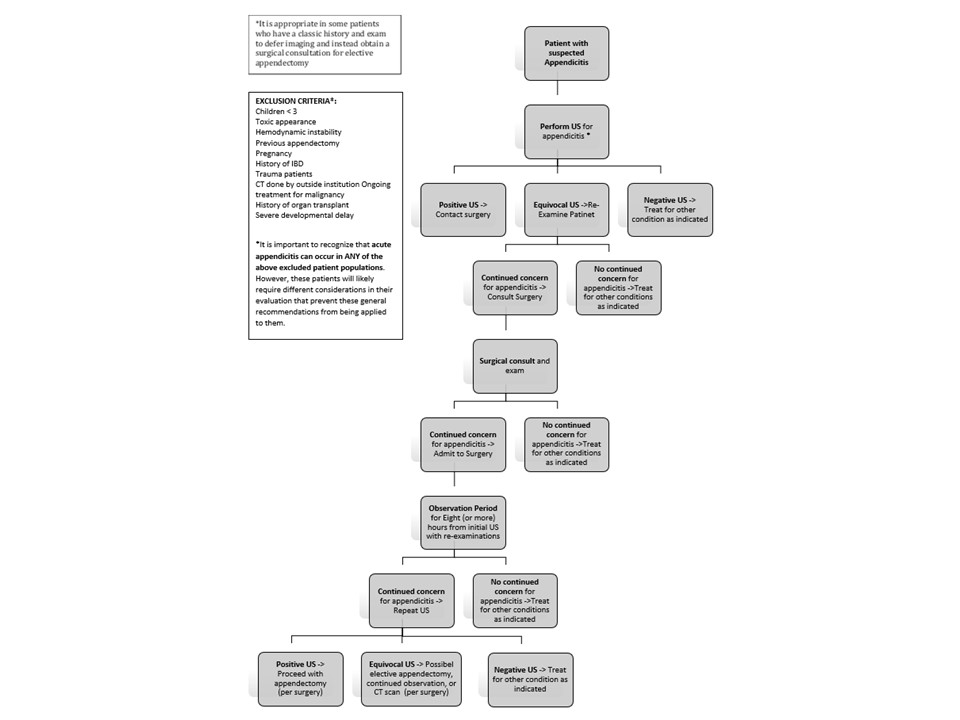
Background: Exposure to ionizing radiation with CT has been potentially associated with increased risk of malignancies in children. CT is typically used to diagnose pediatric appendicitis after an initial US fails to definitively do so, which occurs in as many as 50% of cases. Recently published work has demonstrated that utilizing serial exams and repeat US can obviate the need for CT in many cases without sacrificing diagnostic accuracy.
Objective: The purpose of this quality improvement project was to reduce the utilization of CT to diagnose appendicitis by 75% over a one-year period through implementation of a serial exam and US clinical pathway.
Design/Methods: This is a time series quality improvement project describing baseline data (historical control data) for utilization of CT for the diagnosis of acute appendicitis and demonstrating changes from baseline after the adoption of a serial US clinical pathway.
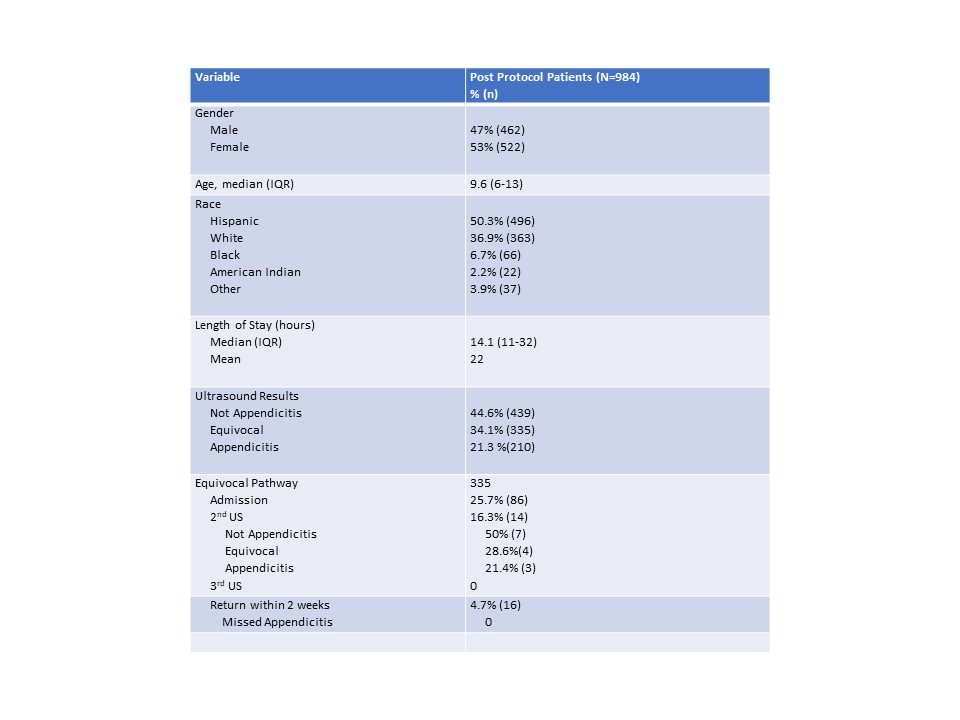
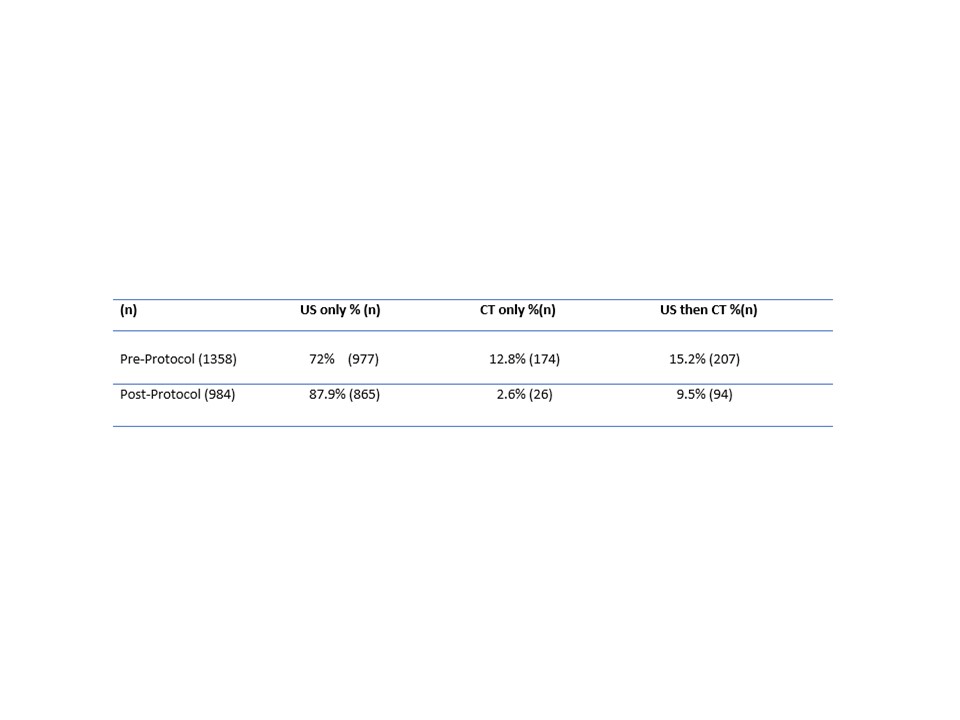
Results: A total of 1,358 pre-protocol patients and 984 post-protocol patients met inclusion criteria. Imaging data of post-protocol patients showed US 44.6% were not appendicitis, 21.3% were appendicitis and 34.1% were equivocal for appendicits. Of the patients with equivocal ultrasounds 74% were discharged home from the emergency department. 6.5% of these patients returned to our ED with complaints of abdominal pain with 0 of these patients having missed appendicitis. 26% of patients with equivocal ultrasounds were admitted with 2.5% of these going to the operating room without additional imaging all of which had confirmed appendicitis on histology and 25% with perforation. Serial US were utilized in 14 patients who received a second US after admission. Of those, 21% had an appendicitis and taken to the OR with histological confirmation. 50% were found to not have appendicitis and 29% were again equivocal. Of those, with a second equivocal US none were taken to the OR and all were able to be discharged. On the evaluation of pre-protocol data 72% were evaluated for appendicitis with US only, 13% CT only, and 15% had US then CT while in the ED. During the post-protocol period 87.9% were evaluated with US only, 2.6% had CT only and 9.5% had US then CT in the ED. There was as statistically significant reduction in CT use post-protocol implementation.
Conclusion(s): Implementation of a serial US pathway resulted in a statistically significant reduction in CT scans through process measures, provider education on CT radiation in pediatrics and multidisciplinary efforts from emergency, surgery, and radiology departments.