Neonatal Clinical Trials
Neonatal Clinical Trials 2
278 - A Randomized Trial of Umbilical or Peripheral Catheter Insertion for Preterm Infants on Admission to the NICU
Publication Number: 278.428
- ED
Emma A. Dunne, MB BCh BAO MRCPI BSc (she/her/hers)
Doctor
National Maternity Hospital, Holles Street, Dublin 2
Dublin 11, Dublin, Ireland
Presenting Author(s)
Background:
While hypothermia on admission to the neonatal intensive care unit (NICU) is an independent risk factor for mortality in preterm infants, less is known about the effect of hypothermia after NICU admission. One study reported that 93% of infants were hypothermic in the three hours following NICU admission. Umbilical venous catheters are commonly inserted in extremely preterm infants on NICU admission. This involves a period of exposure which may increase infants’ risk of hypothermia. One study reported that 89% of infants become hypothermic during umbilical catheterisation.
Objective:
To determine whether placing a peripheral intravenous catheter (PIVC), compared to an umbilical venous catheter (UVC) on admission to the NICU, results in more infants with a temperature in the normal range 2 hours after birth.
Design/Methods:
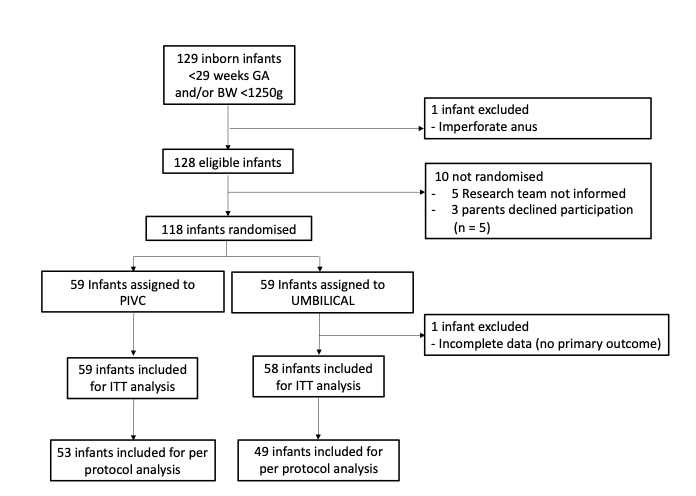
We conducted this randomised trial at a university maternity hospital. Infants born before 29 weeks gestational age (GA) or with a birthweight (BW) < 1250g were eligible for inclusion. Infants with large abdominal wall defects, neural tube defects or imperforate anus were ineligible. Infants were randomly assigned to PIVC or UVC on NICU admission. Caregivers were not masked to group assignment. The primary outcome was rectal temperature in the normal range (36.5oC – 37.5oC) two hours after birth.
Results:
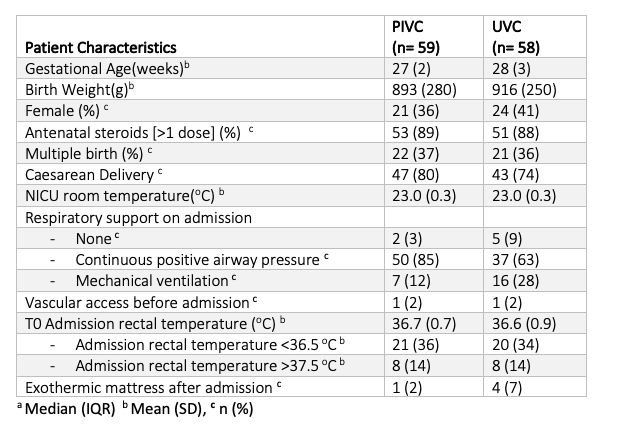
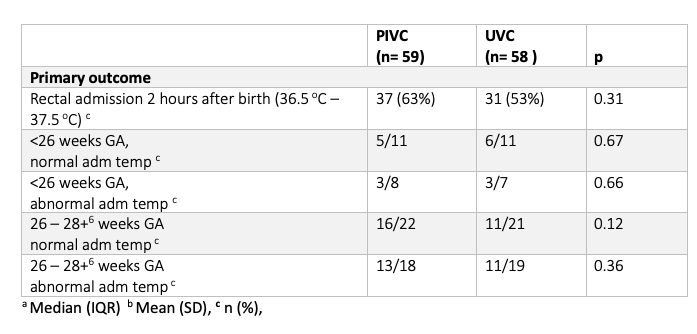
Between March 2021 and November 2022, 118/129 (91%) eligible infants were enrolled to this study; one infant with an imperforate anus was not enrolled. 59 infants were randomly assigned to PIVC (21 [36%] female) and 59 to UVC (24/59 female [41%]). Outcome data was incomplete for one infant, and they were excluded (Fig 1). The mean [SD] GA was 27 [2] vs 28 [9] weeks, and mean [SD] birthweight was 893 [280] vs 916 [250] grams respectively (Table 1). The proportion of infants with a temperature in the normal range two hours after birth was similar between the two groups on intention to treat analysis (PIVC; 37/59 (63%) vs UVC; 31/58 (53%), p 0.31). On per protocol analysis, more infants in the PIVC group had a rectal temperature in the normal range 2 hours after birth, but the difference was not statistically significant (PIVC 35/54 [66%] vs UMBILICAL 24/49 [49%]; RR 0.45 CI 0.22 – 1.1, p 0.08). Ninety-eight (84%) infants had a temperature outside of the normal range in the 2 hours after birth.
Conclusion(s):
Placing a PIVC instead of a UVC on admission, does not result in more infants with a normal temperature 2 hours after birth. Abnormal temperature after admission to the NICU is common in extremely preterm infants. Research into thermoregulation after admission to the NICU is needed.