Neonatal Quality Improvement
Neonatal Quality Improvement 6
205 - Improving Timely and Simultaneous Immunizations in the Neonatal Intensive Care Unit for ELBW Infants
Publication Number: 205.44

Beverly A. Giang, MD (she/her/hers)
Neonatology Fellow
Loma Linda University Children's Hospital
Loma Linda, California, United States
Presenting Author(s)
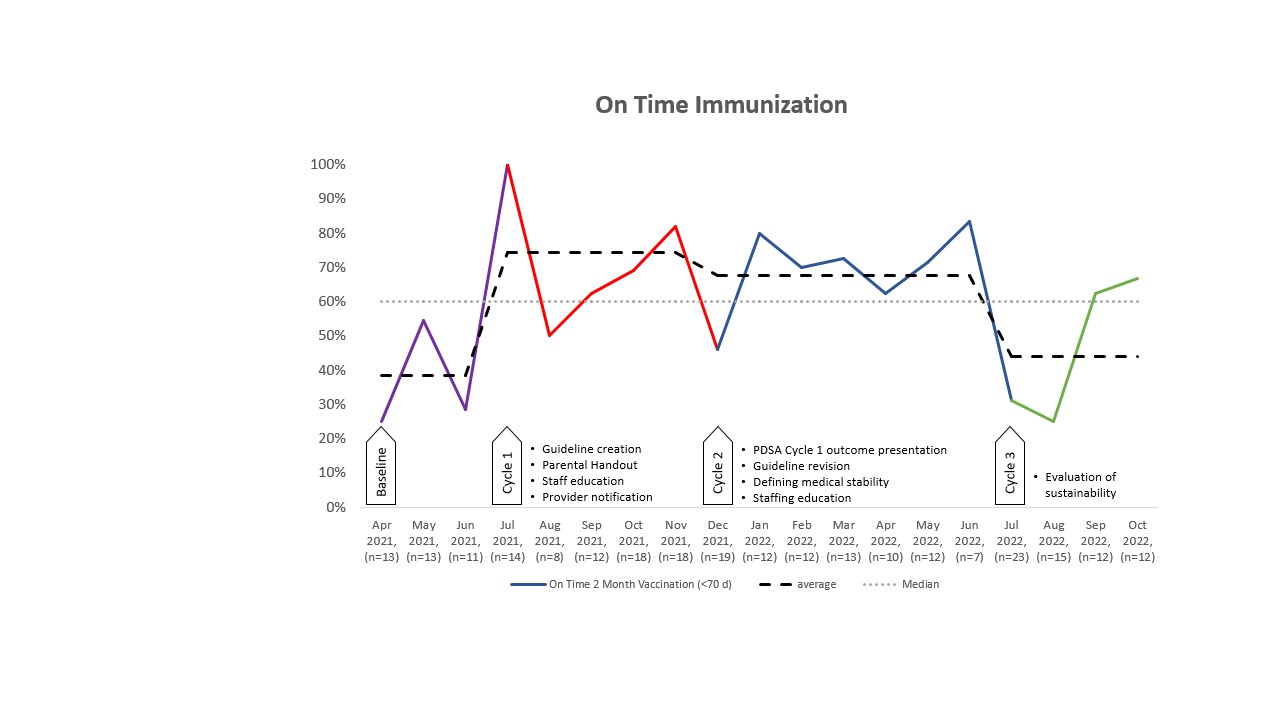
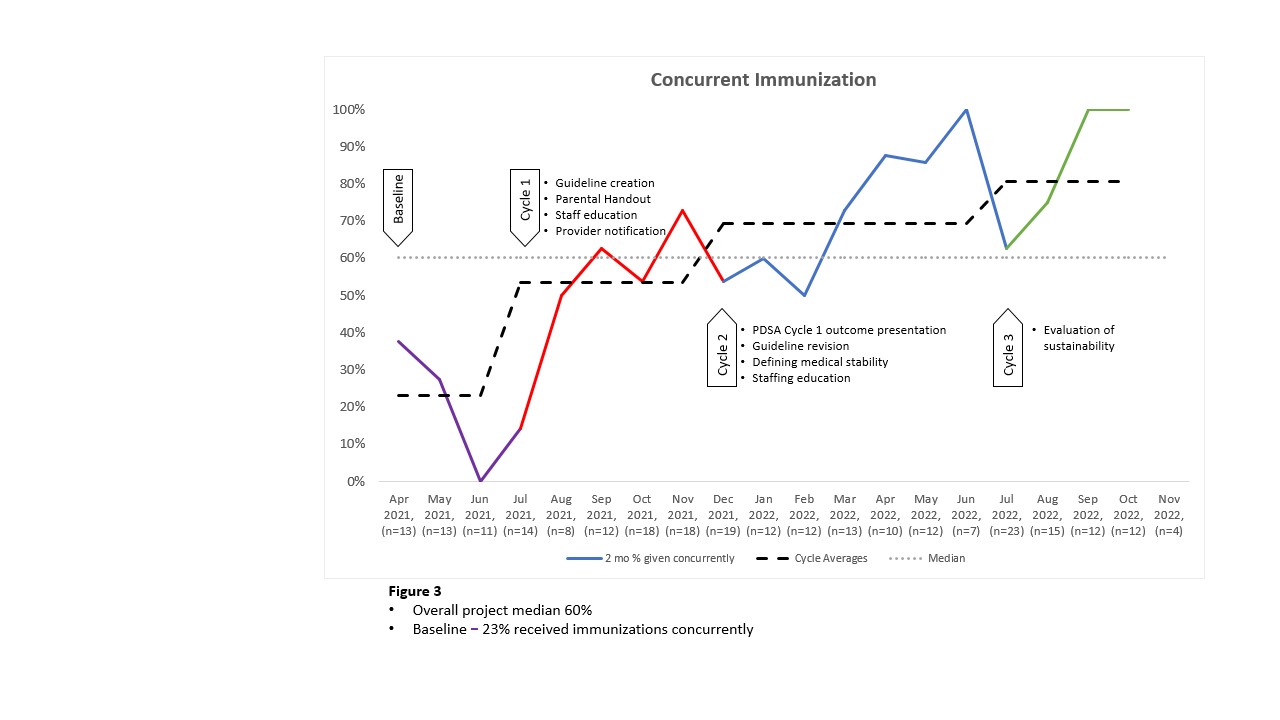
Background: Preterm infants in the NICU are at a high risk of morbidity and mortality from vaccine preventable diseases. Furthermore, delayed or non-immunization is linked to an increased risk for delayed of subsequent immunizations. The American Academy of Pediatrics recommends vaccination of medically stable preterm infants based on chronological age regardless of birth weight or gestational age. From April 2021 to June 2021, only 38% of eligible infants in our single center level IV NICU received two-month immunizations on time (60 days +/- 10 days). In addition, only 23% of infants received immunizations concurrently.
Objective: We aimed to increase the rates of on time and concurrent immunization to 70% within 12 months.
Design/Methods:
Using the Model for Improvement process of Plan, Do, Study, Act (PDSA), we obtained baseline data from our electronic health record. The primary drivers for delayed vaccinations included failure of providers to order vaccines when due, recognition of medical stability for immunization, nursing hesitancy to administer vaccinations concurrently and immunization hesitancy from parents. The project consisted of 2 PDSA cycles with interventions and 1 PDSA cycle to monitor for sustainability of the project. Metrics were collected through identification of eligible infants and chart review of the administration of the immunizations.
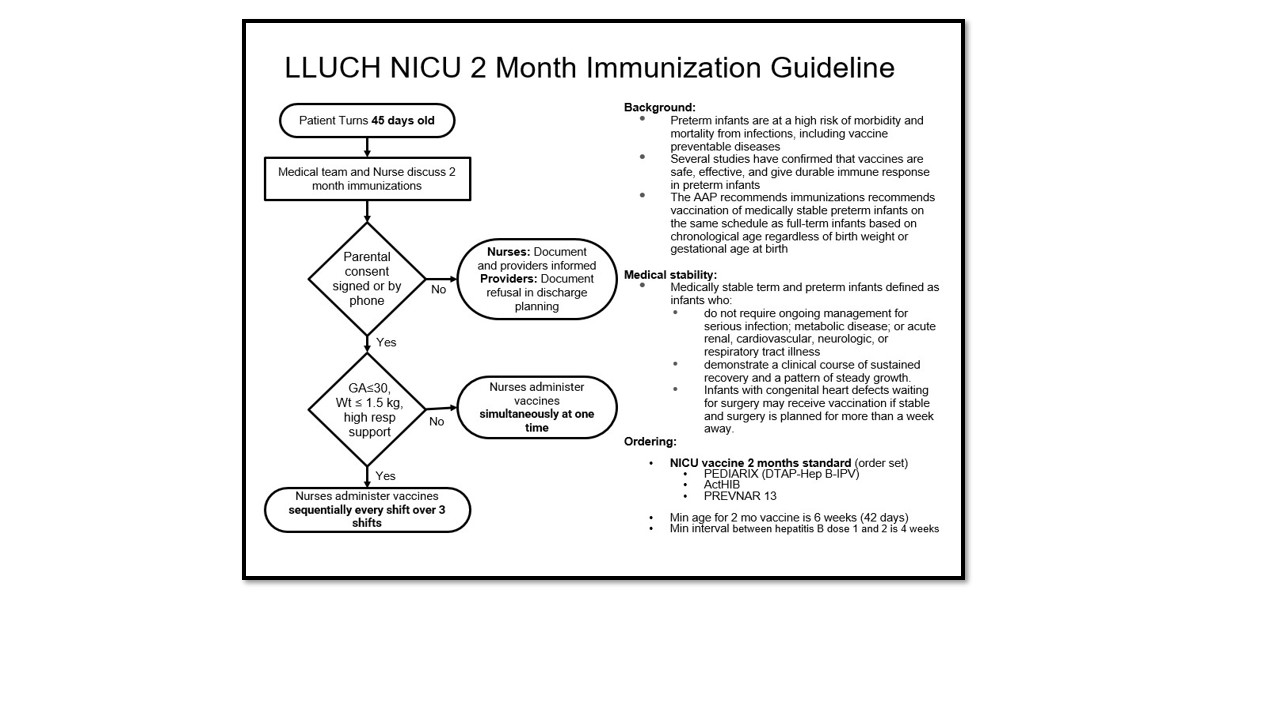
The interventions during the first PDSA cycle included creation of an immunization guideline (Fig 1), staffing education, creation of informational handouts for parents, and notification of eligible patients to providers. The second PDSA consisted in revision of the immunization guideline to clarify the definition of medical stability of patients and continued education of our staff.
Results: The average rate of on time immunizations rose from 38% to 74%, 68% and 44% for our PDSA cycles 1, 2 and 3 (Fig 2). The average rate of vaccines given simultaneously rose from 23% to 53%, 69% and 81% for our PDSA cycles 1, 2, and 3 (Fig 3).
Conclusion(s): The rate of on time and simultaneous immunizations improved significantly in our level IV NICU within 12 months with the implementation of a vaccination guideline and education for providers and parents. These interventions may be useful for other centers with low rates of immunizations. Sustainability was successful for our concurrent administration of immunizations but on time immunization remained a challenge due to acuity and clinical stability of our patients at the time of eligibility.