Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 4: Surfactant and NIV 1
656 - Feasibility of Synchronized High Flow Nasal Cannula in an Animal Model of Lung Injury and an Infant with Bronchopulmonary Dysplasia
Publication Number: 656.442
David N. Matlock, Jr., MD
Assistant Professor
University of Arkansas for Medical Sciences
Little Rock, Arkansas, United States
Presenting Author(s)
Background: High flow nasal cannula (HFNC) is a widely used mode of respiratory support. By design, HFNC delivers continuous flow during inspiration and expiration, which may lead to adverse effects such as dynamic hyperinflation or the baby “fighting” the flow delivered during exhalation. Synchronization of HFNC, whereby high flow is delivered on inspiration only (and low continuous flow during exhalation) has never been evaluated for feasibility. In the present study, we use the electrical activity of the diaphragm (Edi) as a neural controller for synchronizing HFNC (sHFNC), and we compare it to continuous HFNC (cHFNC) in an animal model of lung injury and an infant with bronchopulmonary dysplasia (BPD).
Objective:
To demonstrate feasibility of sHFNC in an animal model of lung injury and an infant with BPD.
Design/Methods:
Animal study: Eight rabbits (mean weight 3.16 kg) were studied before and after HCl-induced acute lung injury (ALI) using a prototype ventilator capable of delivering both cHFNC and sHFNC via a single nasal prong (2.5 mm inner diameter). The following conditions were tested before and after ALI for 5 minutes each: baseline (no assist), 4 LPM, 6 LPM, 8 LPM, and 10 LPM. Expiratory flow during sHFNC was always 2 LPM. Arterial blood gases were obtained at the end of each 5 minute period. We measured Edi and pressures at the prong (Pprong), esophagus (Pes), and stomach (Pga).
Infant study: After obtaining parental consent, one infant with BPD was studied using a RAM™ cannula and Servo-U ventilator in the non-invasive neurally adjusted ventilatory assist (NIV NAVA) mode set to maximum NAVA level (15) with a pressure limit providing 8 LPM flow on inspiration and 2 LPM on exhalation and then using 8 LPM continuous flow for 10 minutes each.
Results:
Animal study: As illustrated in table 1 and figure 1, during both cHFNC and sHFNC, there were pronounced decreases in Edi and Pes swings as flow level increased, which were more pronounced during sHFNC (p< 0.05 pre and post ALI). PaCO2 reductions were greater for sHFNC at 6, 8, and 10 LPM pre ALI and at 10 LPM post ALI. Baseline Pes (i.e. end expiratory value) was 1-2 cmH2O greater during cHFNC than sHFNC indicating more dynamic hyperinflation during the continuous mode.
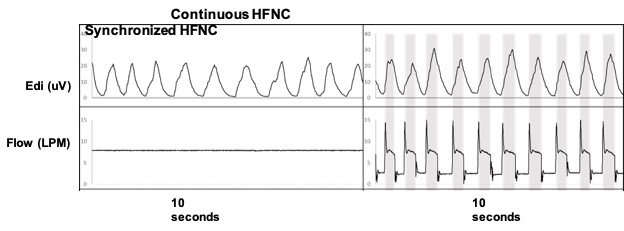
Infant study: In one 107 day old, 3.52 kg, male infant with BPD and tracheomalacia, the Servo-U performed as expected, demonstrating feasibility of synchronizing HFNC in human infants (Figure 2).
Conclusion(s):
sHFNC decreased Edi in an animal model and is feasible in an infant with BPD. Further investigation of this method of support, especially for infants with BPD is warranted.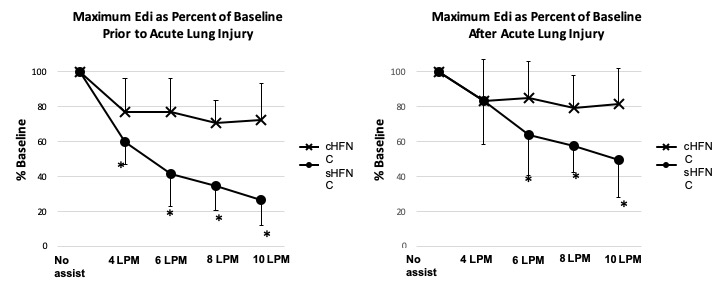
.jpg)
