Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 3
686 - Missing the mark: Standard endotracheal tube depth estimates are too shallow in patients with Congenital Diaphragmatic Hernia
Publication Number: 686.444

Allison C. Young, MD (she/her/hers)
Resident
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Initial resuscitation of infants with Congenital Diaphragmatic Hernia (CDH) includes immediate intubation to manage respiratory failure and facilitate decompression. Estimating correct endotracheal tube (ETT) depth prior to intubation is necessary to reduce complications and provide adequate respiratory support. However, the ideal ETT depth in infants with CDH may be affected by displacement of the airway by intrathoracic abdominal viscera. Thus, previously established strategies to predict ETT depth may be suboptimal in this population.
Objective:
To compare the clinically preferred ETT depth in infants with CDH to predicted depths using the weight-based and Neonatal Resuscitation Program (NRP) gestational age-based estimates.
Design/Methods:
This single-center, retrospective study included inborn infants with left-sided CDH born from January 2017 to August 2022. Patients who underwent fetal intervention or with skeletal anomalies were excluded. Extracted data included patient characteristics, indices of CDH severity, initial radiographs, and details of ETT management. On radiographs, the distance from the tip of the ETT to the level of the T2, T3, and T4 inferior endplates was measured. A standard anatomic depth was calculated by adding the measured displacement to T2 to the initial ETT depth. Predicted depths were estimated using the weight + 6cm formula and NRP recommendations based on gestational age. Paired t-tests were used to compare both final clinical depth at 24 hours of life and calculated standard anatomic depth to the initial predicted depths.
Results:
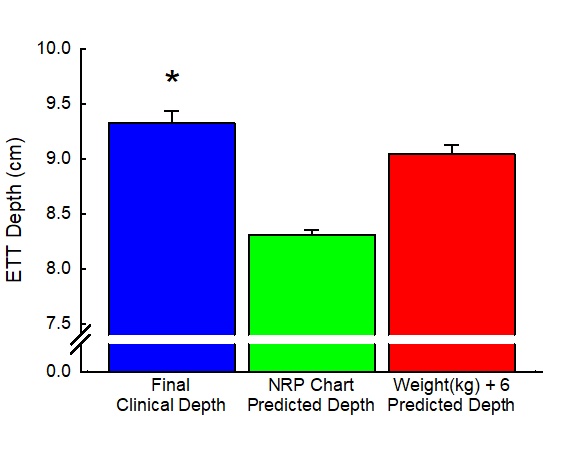
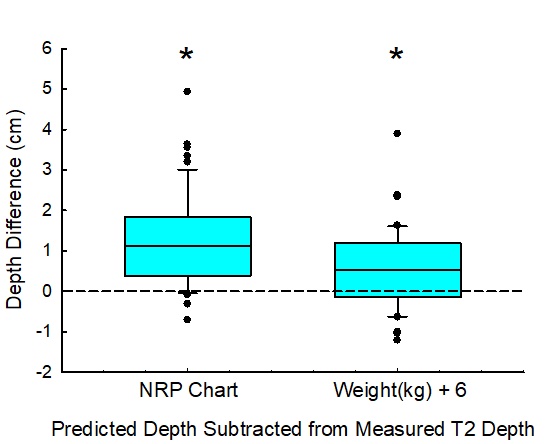
Of the 58 infants included, 43% required ETT advancement by the end of day one of life in contrast to the 24% requiring retraction. 29% of the initial ETT placements were at or above the thoracic inlet. The clinically preferred ETT depth was on average 1.01cm (±0.77, std dev) deeper than the NRP age-based estimate (p< 0.001) and 0.26cm (±0.50, std dev) deeper than the weight-based estimate (p< 0.001, Figure 1). Additionally, the standard anatomic depth was on average 1.3cm deeper than the NRP age-based estimate (p< 0.001) and 0.6cm deeper than the weight-based estimate (p< 0.001, Figure 2).
Conclusion(s):
These discrepancies suggest that previously established strategies to predict ETT depth underestimate the ideal depth in infants with left-sided CDH. The data suggest modifying the current weight-based prediction formula from weight + 6cm to weight + 6.5cm. Further prospective studies are needed to determine whether this alternate approach would reduce the need for ETT adjustment after initial intubation of infants with CDH.