Global Neonatal & Children's Health
Global Neonatal & Children's Health 3
535 - Impact of Social Determinants of Health on Mortality and Morbidity of Pediatric Trauma Patients in Northern Tanzania
Publication Number: 535.409

Natalie J. Tedford, MD (she/her/hers)
Pediatric Emergency Medicine & Global Health Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
Trauma is a leading cause of death and disability in children worldwide, and social determinants of health (SDH) contribute to health outcomes. Limited data exists on the impact of SDH related to health outcomes of children experiencing injuries from trauma in low- and middle-income countries (LMICs).
Objective:
To assess the association in measures of SDH on morbidity and mortality for children experiencing injuries at a referral hospital in an LMIC
Design/Methods:
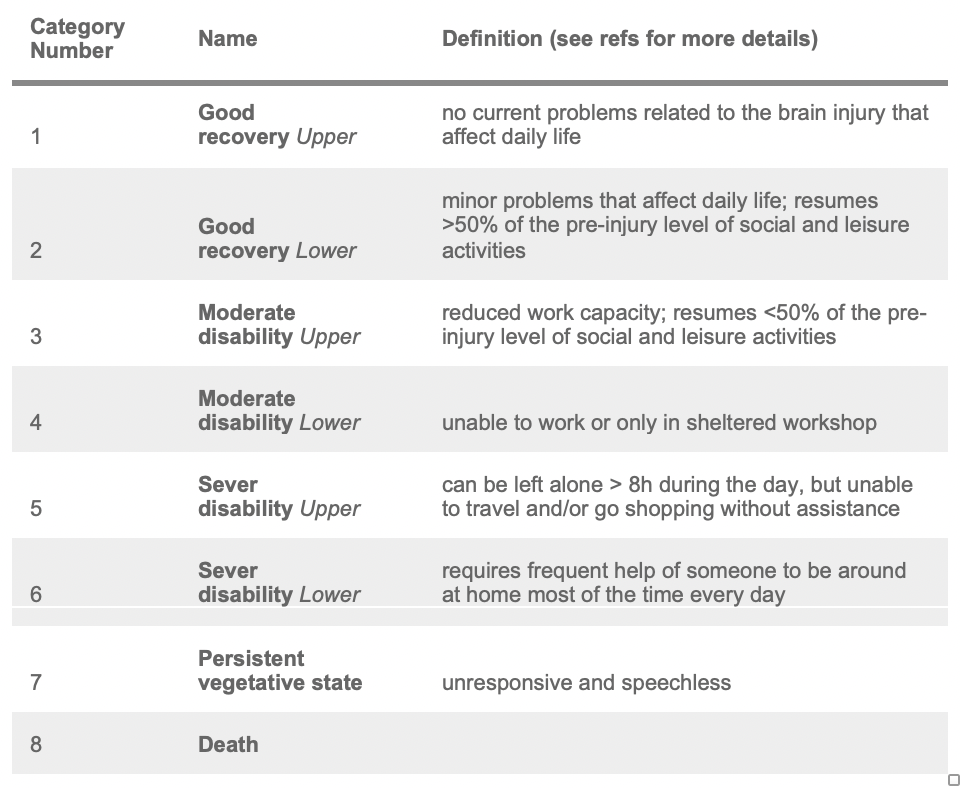
This was a cross-sectional, descriptive study using a prospective pediatric trauma registry at a tertiary hospital in Northern Tanzania. Patients were enrolled in the registry upon presentation to the Emergency Department if they were less than 18 years old and presented with an acute injury. SDH factors collected included: type of community where patient lives, payment method, insurance status, family household makeup, daily nutrition, and mechanism of arrival. Morbidity was measured using the Glasgow Outcome Scale Extended Peds (GOS-E Peds, Table 1). Outcomes of interest were mortality and morbidity. We used Chi-square analysis and risk ratios to assess the association between SDH burden and patient-specific outcomes with attributable fraction (AF) denoted to measure effect of negative SDH factors on outcomes.
Results:
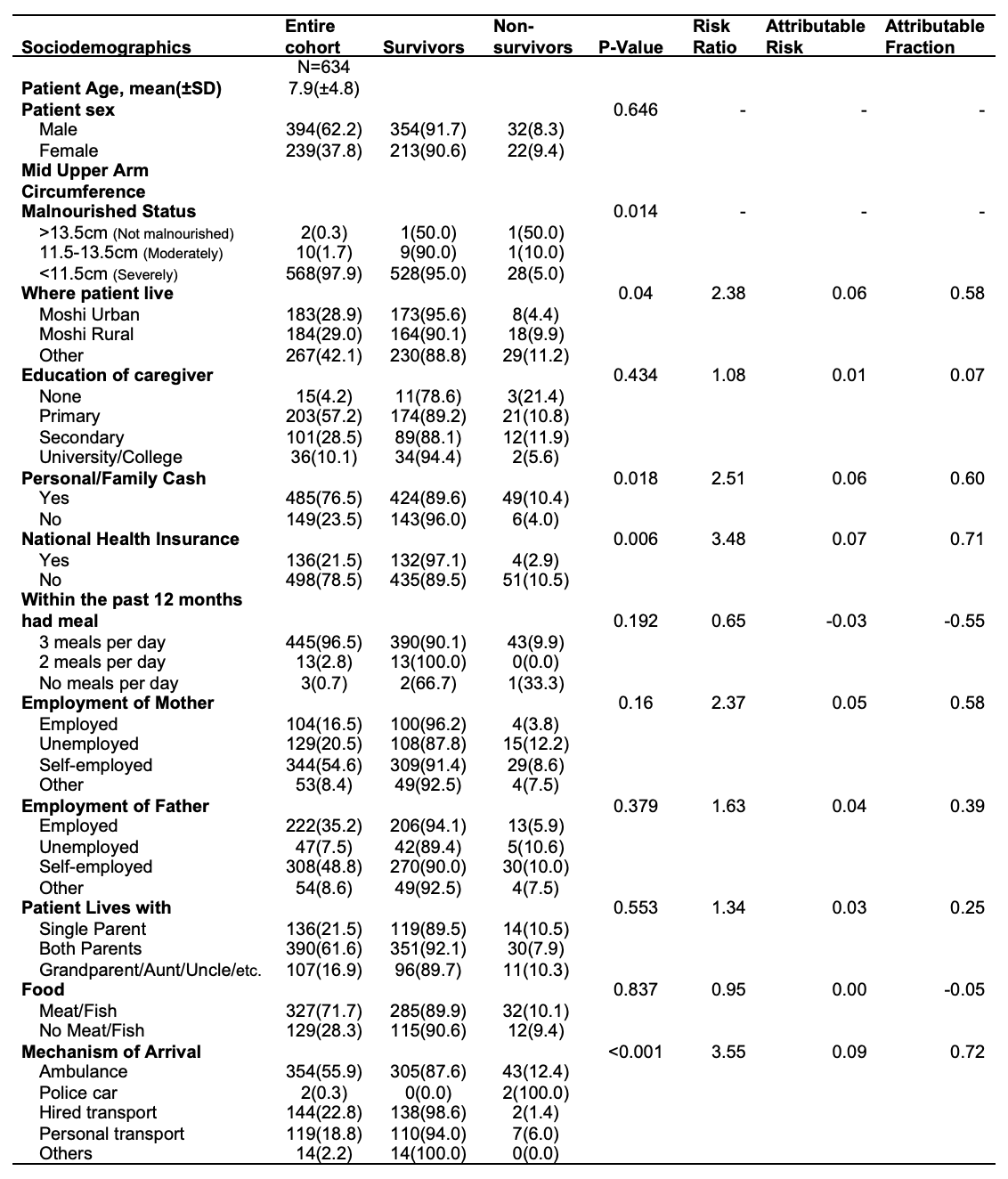
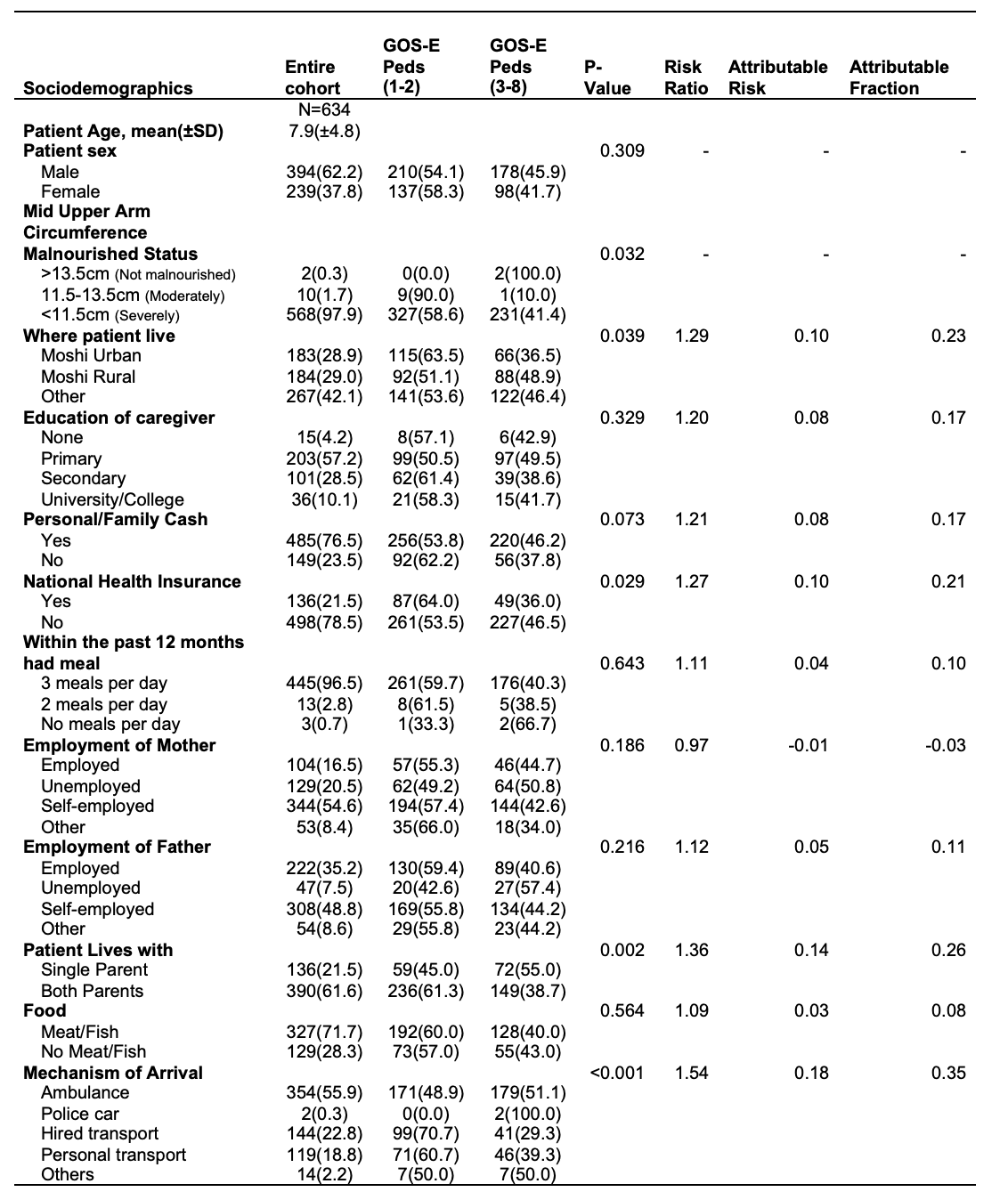
From 11/2020 to 11/2022, 634 patients were enrolled. The majority were males (n=394, 62%), mean age was 7.9 (±4.8) years, and were malnourished (n=578, 99.7%). The mortality rate was 8.5%. Most families paid for care with personal/family cash (n=485, 76.5%), and only 21.5% had National Health Insurance (NHI). Mortality rates were significantly higher (p< 0.05) for patients: not living in Urban Moshi (AF=0.58); personal/family cash for payment (AF=0.6); and lacked NHI (AF=0.71) (Table 2). Morbidity at discharge (GOS-E Peds score ³ 3) was significantly higher (p,0.05) for patients: not living in Urban Moshi (AF=0.23); lacked NHI (AF=0.21); and do not live with both parents (AF=0.26) (Table 3). Patients whose mechanism of arrival was via personal or hired transport had statistically lower (p< 0.001) mortality (AF=0.71) and morbidity (AF=0.35) at discharge.
Conclusion(s):
Our study found several SDH factors that were associated with higher mortality and morbidity with effect being greatest when evaluating mortality outcomes. This analysis highlights the importance of understanding SDH-related impacts on patient outcomes and integrating inequality monitoring into the health information system in LMICs. Next steps would be interventions that help address and minimize SDH burden for patients with injuries during hospitalization.