Neonatal Quality Improvement
Neonatal Quality Improvement 6
204 - Quality Improvement Project to Decrease Unplanned Extubations Utilizing Simulation and Visual Tools in a Level IV Neonatal Intensive Care Unit
Publication Number: 204.44
- HA
Hamza F. Abbasi, MBBS (he/him/his)
Fellow physician
University at Buffalo
east amherst, New York, United States
Presenting Author(s)
Background:
Unplanned extubations (UE) are preventable events in the NICU. Adverse outcomes are associated with UEs, including neonatal mortality, significant hemodynamic instability, temperature instability, prolonged hospital length of stay, airway trauma/subglottic We significantly decreased monthly UEs/100 ventilator days by implementing an evidence-based protocol supported with simulation sessions and visual tools. We continue our initiative to bring it further down to < 1/100 vent days.
stenosis, and ventilator-associated pneumonia. Our NICU did not have a consistent process to track UEs and minimize their occurrence.
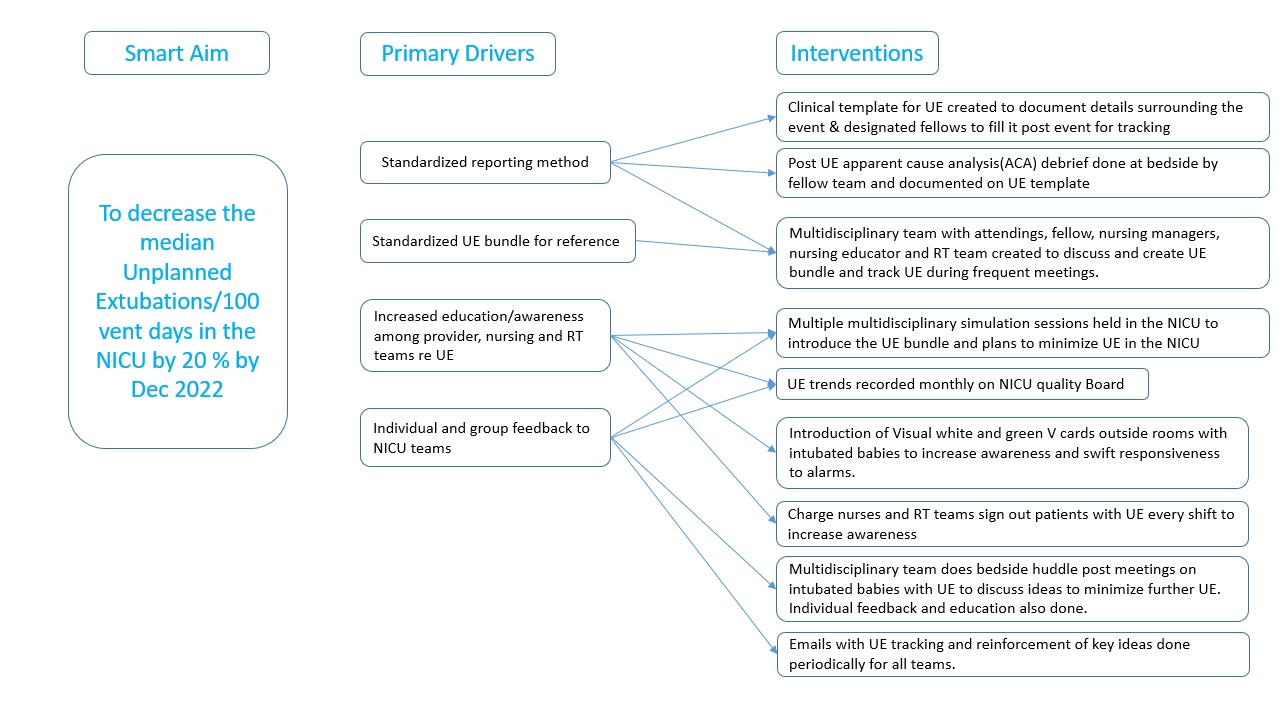
Objective: To decrease the median incidence of UE/100 vent days by 20% by December 2022 in a level IV NICU, utilizing Visual Tools and
case-based simulation sessions to implement evidence-based strategies.
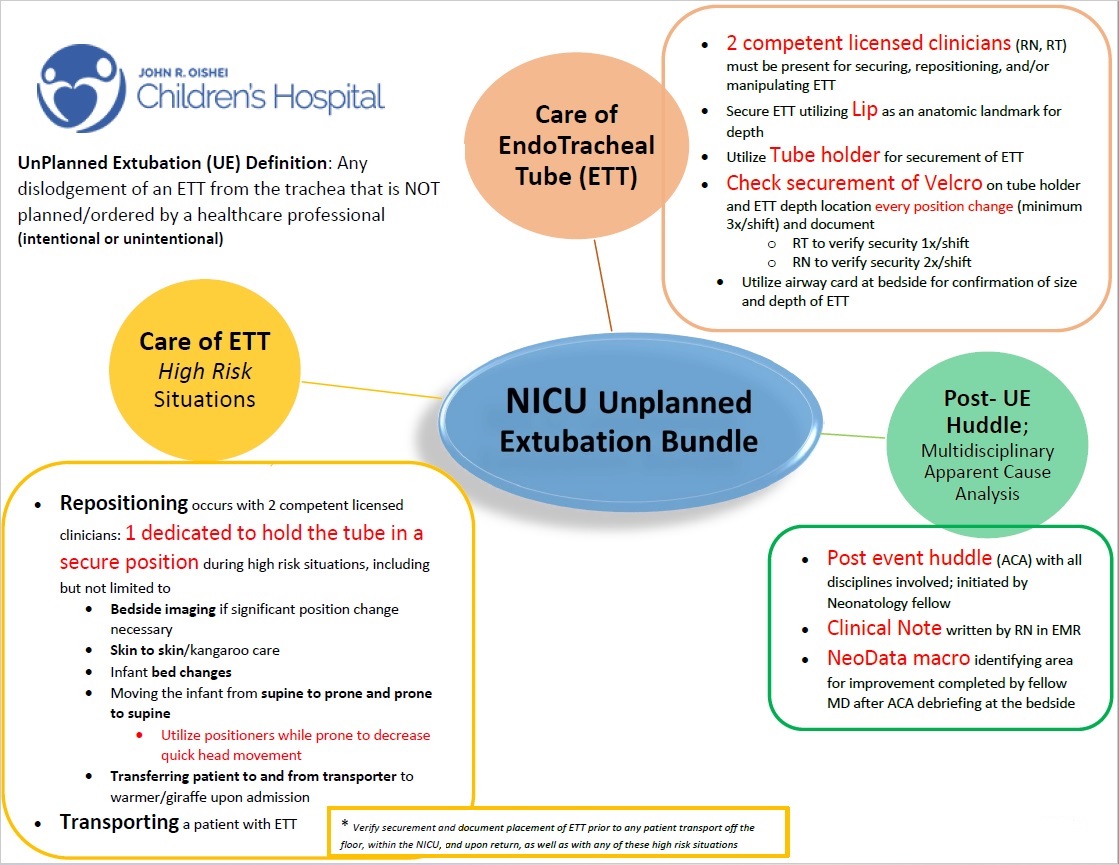
Design/Methods: A multi-disciplinary QI team of Physicians, Nursing and Respiratory therapists was created in October 2020 and standardized template and processes were created for documentation of UEs. Data driven Pareto chart was created to assess common causes and Key Driver-diagram was made based on discussions by the multidisciplinary team (Fig 1). UE reduction care bundle (Fig 2) was designed based on the pareto charts and evidence-based recommendations. Multiple multidisciplinary case-based simulation sessions were led in the NICU in the following months to create awareness around identifying UEs and preventing them by utilizing the bundle infographics. Post UE bedside debriefs were led by fellows to discuss factors leading to UE and plans to prevent another one. UE data was shared every shift by Charge nurses and RTs and the numbers were trended on the Quality board in the NICU. Multiple PDSA cycles were run to minimize UE amidst the p</span>andemic and staffing challenges. Visual Signage with a white “V” Card
was created and placed on the doors of ventilated patients to increase awareness and responsiveness to alarms for that room, while green colored “V” cards were placed for those with >1 UE for heightened vigilance. Near-term NICU patients with UEs were transitioned to taping instead of usual ETT securement device. The multidisciplinary team met frequently to discuss UEs and gave individual/group feedback to team members.
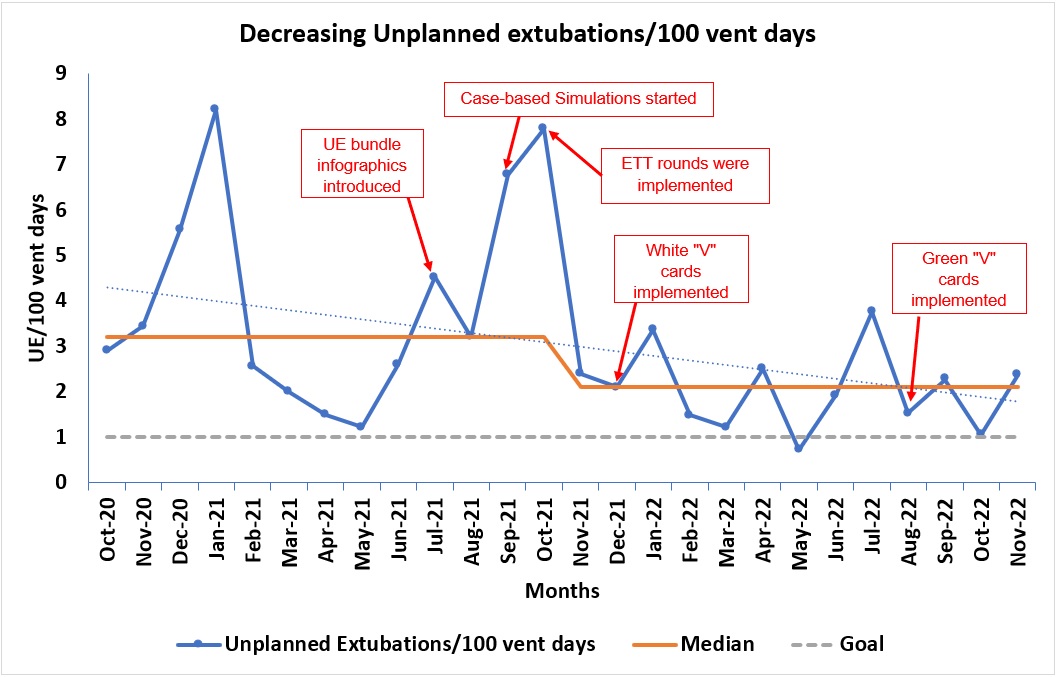
Results: We decreased the median incidence of UE/100 vent-days by 30% by December 2022(Graph 1). This was despite an upward trending total ventilator days per month over time. There was a statistically significant decrease between the time period 10/2020-10/2021 (4.02+/-2.36; median 3.21) and 11/2021-11/2022 (2.05+/-0.87; median 2.1), P=0.009.
Conclusion(s):