Back
Background: Hypothermia on admission to the neonatal intensive care unit (NICU) increases preterm infants’ risk of death. Preterm infants are placed in polyethylene bags (PB) after umbilical cord clamping (CC) to reduce heat loss. Delayed CC is now recommended for preterm infants. Delay in putting preterm infants in PB may increase their risk of hypothermia.
Objective: To determine whether placing very preterm infants in a PB before CC, compared to after CC, results in more infants with a temperature in the normal range on NICU admission.
Design/Methods: We conducted a randomized controlled trial at a tertiary maternity hospital (c. 100 births < 32 weeks’ gestational age [GA] per annum). Infants were stratified by gestational age (GA), and were enrolled with prospective consent when circumstances permitted, or with deferred consent when they didn’t. Participants were followed until death or discharge. Infants < 32 weeks’ GA for whom intensive care was planned were eligible for inclusion. Infants were excluded if they had an imperforate anus, abdominal wall or neural tube defects. Infants were randomly assigned to have a PB placed before or after CC. Caregivers were not masked to group assignment. The primary outcome was rectal temperature within the normal range (36.5oC – 37.5oC) on NICU admission.
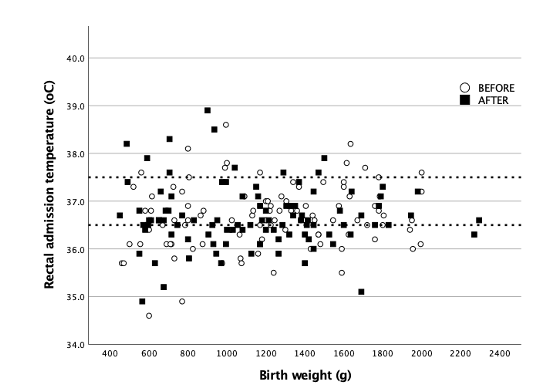
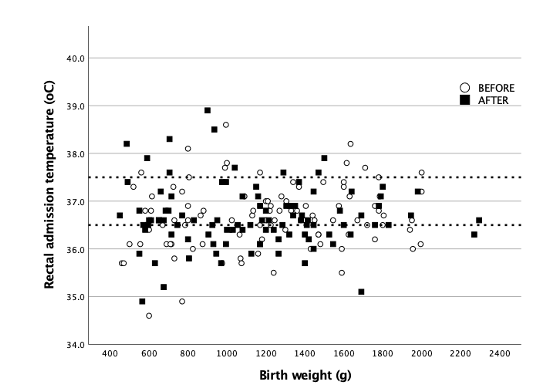
Results: Between July 2020 – September 2022, 198/220 (90%) eligible infants were enrolled to this study; 99 were randomly assigned to BEFORE (44 [44%] female) and 99 (53 [54%] female) to AFTER. The primary outcome was not recorded one of whom died in the delivery room (DR). Data from 197 infants were analysed; the median [IQR] GA was 29 [27,31] vs 29 [27,31] weeks, and mean [SD] birthweight was 1200 [426] vs 1138 [419] grams respectively. The groups were well matched for patient characteristics at study entry.[table 1] The proportion of infants who had normal temperature on NICU admission did not differ between the groups (BEFORE 54/99 [54%] vs AFTER 55/98 [56%]; RR 0.98, 95% CI 0.77 – 1.27, p 0.886). The proportion of infants with a temperature outside of the normal range was similar between the groups; hypothermia (BEFORE 34/99 [34%] vs AFTER 33/98 [34%], p 0.880), hyperthermia (BEFORE 10/99 [10%] vs AFTER 10/98 [10%], p 1.00)[Figure 1]. There were no significant differences in secondary outcomes between the groups [Table 2].
Conclusion(s): Placing a PB before CC did not increase the proportion of preterm infants with normal temperature on NICU admission. A large proportion of preterm infants had abnormal temperature at NICU admission. Further studies on thermoregulation before CC are needed.
.png)
.png)
Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 3
692 - Placing Preterm Infants in Polyethylene Bags Before Umbilical Cord Clamping: A Randomised Trial
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 692
Publication Number: 692.444
Publication Number: 692.444
Emma A. Dunne, National Maternity Hospital, Holles Street, Dublin 2, Dublin 11, Dublin, Ireland; Caitríona M Ní Chathasaigh, The National Maternity Hospital, Dublin, Ireland, Dublin 8, Dublin, Ireland; Lucy E. Geraghty, National Maternity Hospital, Dublin, Dublin, Ireland; Colm P.F.. O'Donnell, National Maternity Hospital & University College Dublin, Ireland, Dublin, Dublin, Ireland; Lisa K. McCarthy, University College Dublin, Dublin, Dublin, Ireland
- ED
Emma A. Dunne, MB BCh BAO MRCPI BSc (she/her/hers)
Doctor
National Maternity Hospital, Holles Street, Dublin 2
Dublin 11, Dublin, Ireland
Presenting Author(s)
Background: Hypothermia on admission to the neonatal intensive care unit (NICU) increases preterm infants’ risk of death. Preterm infants are placed in polyethylene bags (PB) after umbilical cord clamping (CC) to reduce heat loss. Delayed CC is now recommended for preterm infants. Delay in putting preterm infants in PB may increase their risk of hypothermia.
Objective: To determine whether placing very preterm infants in a PB before CC, compared to after CC, results in more infants with a temperature in the normal range on NICU admission.
Design/Methods: We conducted a randomized controlled trial at a tertiary maternity hospital (c. 100 births < 32 weeks’ gestational age [GA] per annum). Infants were stratified by gestational age (GA), and were enrolled with prospective consent when circumstances permitted, or with deferred consent when they didn’t. Participants were followed until death or discharge. Infants < 32 weeks’ GA for whom intensive care was planned were eligible for inclusion. Infants were excluded if they had an imperforate anus, abdominal wall or neural tube defects. Infants were randomly assigned to have a PB placed before or after CC. Caregivers were not masked to group assignment. The primary outcome was rectal temperature within the normal range (36.5oC – 37.5oC) on NICU admission.
Results: Between July 2020 – September 2022, 198/220 (90%) eligible infants were enrolled to this study; 99 were randomly assigned to BEFORE (44 [44%] female) and 99 (53 [54%] female) to AFTER. The primary outcome was not recorded one of whom died in the delivery room (DR). Data from 197 infants were analysed; the median [IQR] GA was 29 [27,31] vs 29 [27,31] weeks, and mean [SD] birthweight was 1200 [426] vs 1138 [419] grams respectively. The groups were well matched for patient characteristics at study entry.[table 1] The proportion of infants who had normal temperature on NICU admission did not differ between the groups (BEFORE 54/99 [54%] vs AFTER 55/98 [56%]; RR 0.98, 95% CI 0.77 – 1.27, p 0.886). The proportion of infants with a temperature outside of the normal range was similar between the groups; hypothermia (BEFORE 34/99 [34%] vs AFTER 33/98 [34%], p 0.880), hyperthermia (BEFORE 10/99 [10%] vs AFTER 10/98 [10%], p 1.00)[Figure 1]. There were no significant differences in secondary outcomes between the groups [Table 2].
Conclusion(s): Placing a PB before CC did not increase the proportion of preterm infants with normal temperature on NICU admission. A large proportion of preterm infants had abnormal temperature at NICU admission. Further studies on thermoregulation before CC are needed.
.png)
.png)
