Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
91 - Incidence and Risk Factors for Tube-Feeding at Discharge in Infants Following Congenital Heart Disease Surgery - A Single Center Cohort Study
Publication Number: 91.425

Sreekanth Viswanathan, MD, MS (he/him/his)
Associate Professor
Nemours Children's Hospital
Nemours Children’s Hospital
Orlando, Florida, United States
Presenting Author(s)
Background: Congenital heart disease (CHD) is the most common birth defect in the United States. Following surgical repair, many infants with CHD do not develop the skills to feed orally enough to meet their energy demands and are discharged home on gastrostomy tube (G-tube) or nasogastric feeds.
Objective: To determine the incidence and risk factors for tube-feeding at discharge following CHD surgery in the first 6 month of life.
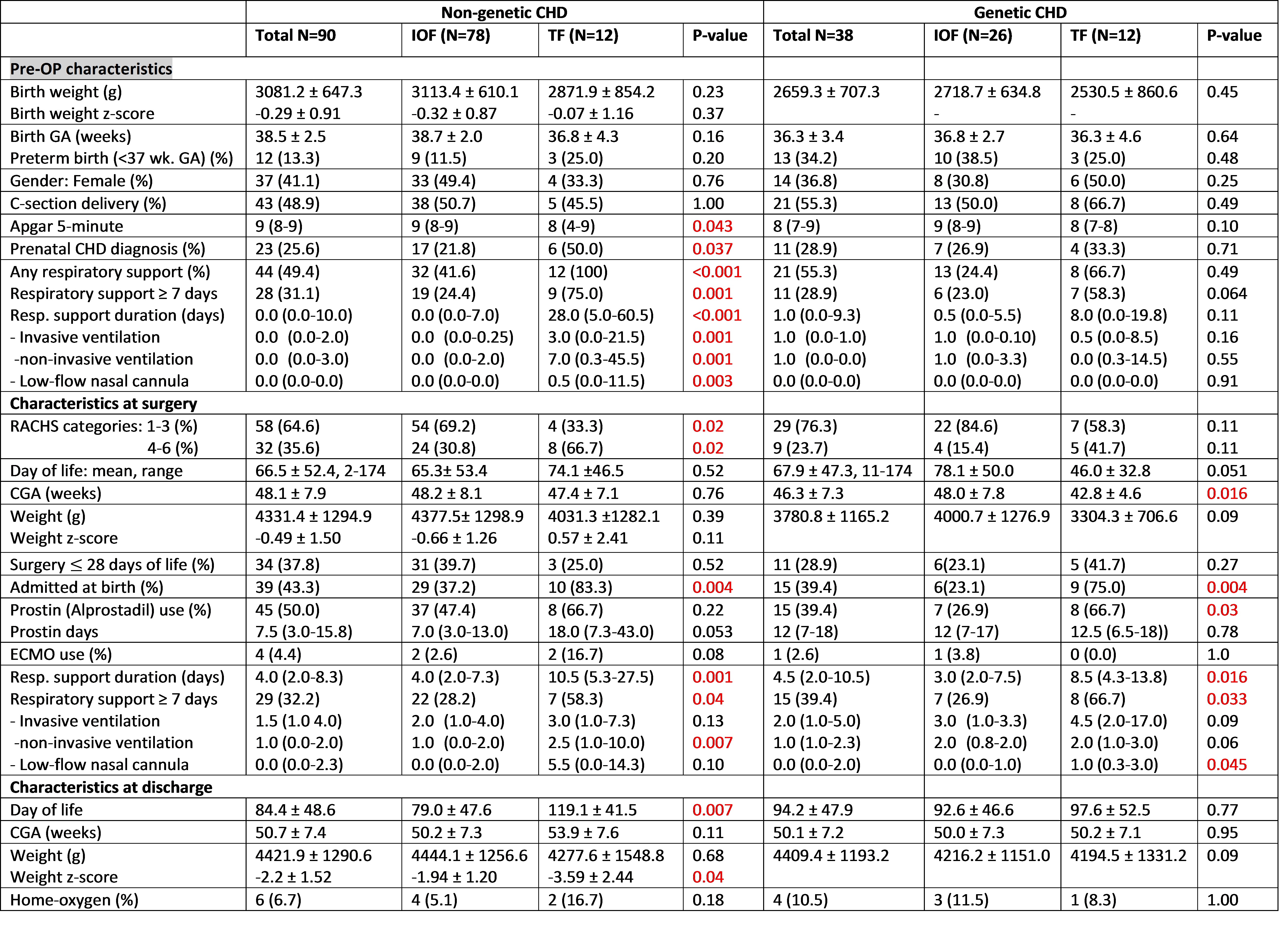
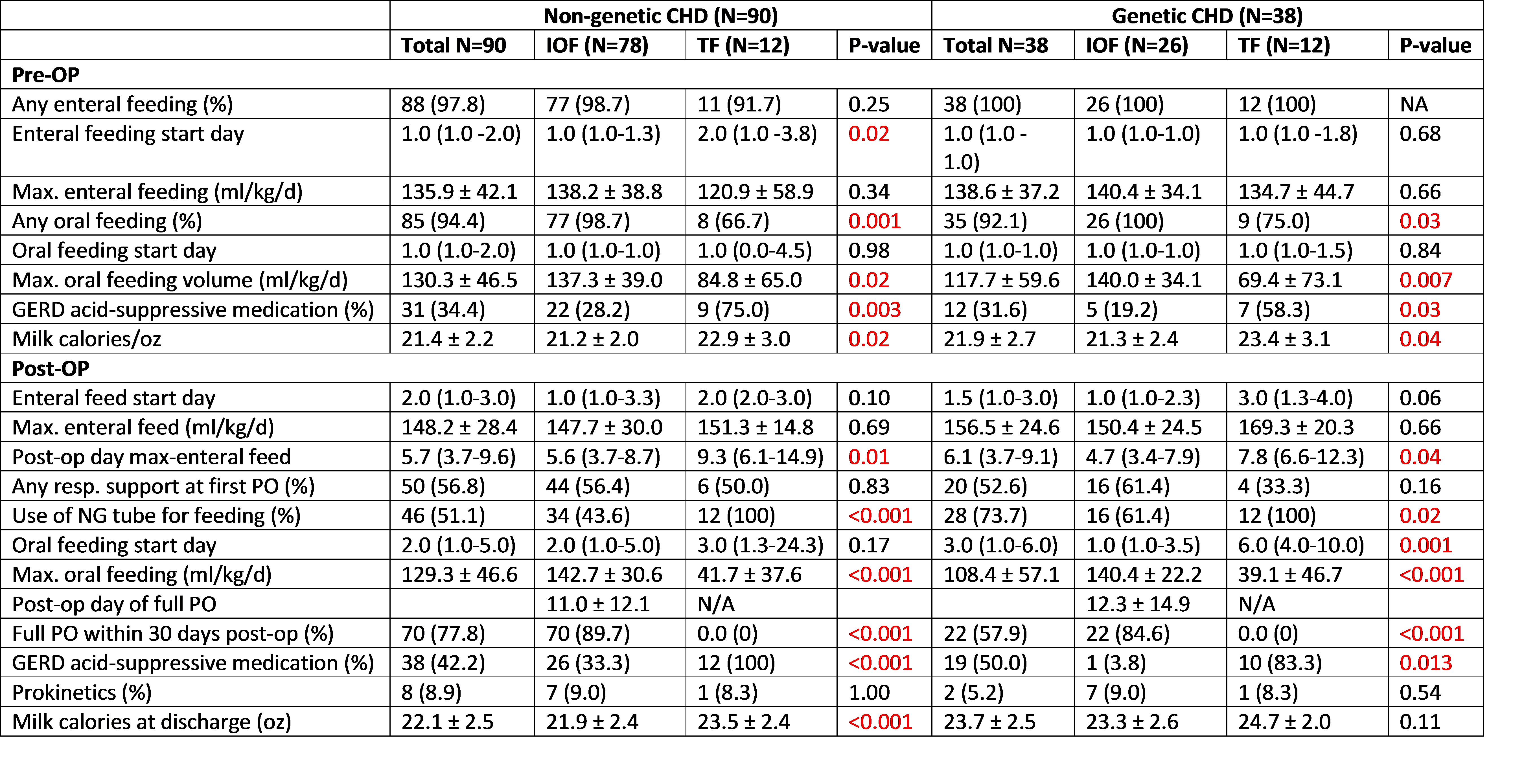
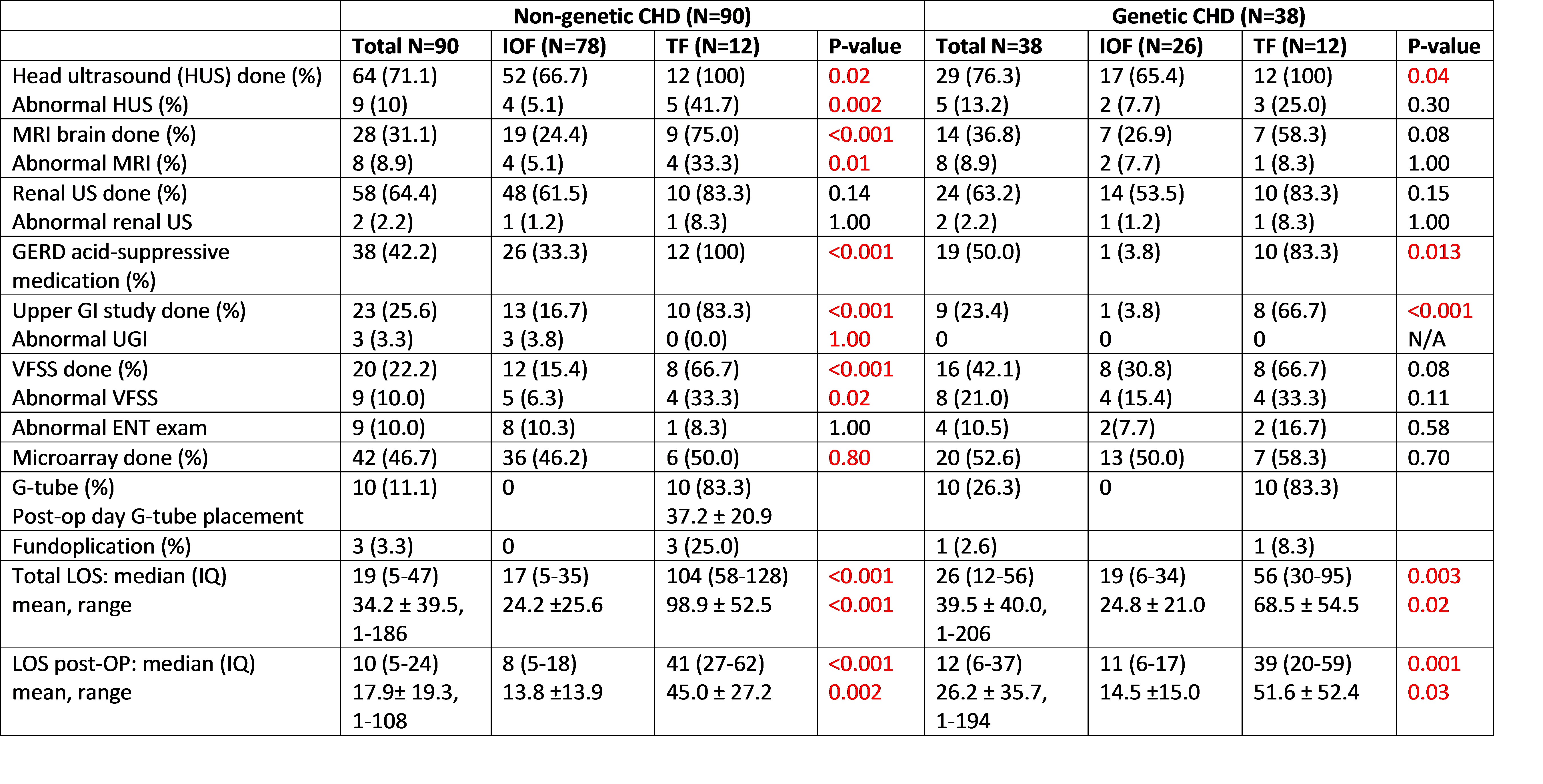
Design/Methods: This was a 6-year single-center retrospective cohort study (Jan 2016 to Dec 2021) conducted at Nemours Children’s Hospital, Orlando, Florida. Charts of infants < 6 months of age who had surgery for CHD were reviewed and separated into two groups: non-genetic CHD and genetic CHD. Infants required tube-feeding at discharge (TF group) were compared to infants who reached independent oral feeding (IOF group) prior to first hospital discharge in both groups. Main exclusion criteria included PDA ligation < 33 weeks corrected gestation, infants who died before reaching IOF or had G-tube before CHD surgery.
Results:
Of the final sample size of 128 infants (non-genetic CHD=90, genetic-CHD=38), 24 (18.8%) infants required TF at discharge [12 each in non-genetic (13.3%) and genetic-CHD (31.6%)]. In the non-genetic CHD, the main independent risk factors for TF include were prenatal CHD diagnosis, risk adjustment for congenital heart surgery (ROCHS) 4-6, pre-op respiratory support ≥ 7 days, post-op respiratory support ≥ 7 days, admitted at birth, pre-op any oral feeding, post-op-gastroesophageal reflux disease (GERD), and abnormal brain MRI (p< 0.05). In the multivariate analysis, only admitted at birth and pre-op respiratory support ≥ 7 days were significant predictors. In the genetic-CHD, risk factors include were corrected gestation at surgery, post-op respiratory support ≥ 7 days, admitted at birth, pre-op any oral feeding, post-op-GERD, and post-op oral feeding start day (p< 0.05). In the multivariate analysis, only admitted at birth and post-op GERD were significant predictors. TF group had significantly higher length of stay (LOS) compared to IOF group in both non-genetic (104 vs. 17 days) and genetic (56 vs.19 days) CHD (p< 0.05).
Conclusion(s):
The incidence of tube-feeding at discharge in our study is comparable to previous studies. The increased LOS in the tube-feeding group reflect the associated increase in health care costs. Mitigating the effects of identified risk factors associated with delayed oral feeding will have significant impact on the quality of life for these infants and their families along with reduction in healthcare cost.