Neonatal Pulmonology
Neonatal Pulmonology 6: Oxygen, Steroids
160 - Association between timing of postnatal dexamethasone initiation and outcomes in very preterm infants with prolonged ventilation: a multi-center cohort study
Publication Number: 160.438
Wenli Li, Master
Associate chief physician
The Third Affiliated Hospital of Zhengzhou University
zhengzhou, Henan, China (People's Republic)
Presenting Author(s)
Background:
Postnatal dexamethasone (PND) is often used to prevent severe bronchopulmonary dysplasia (sBPD) in very preterm infants (VPI) requiring prolonged invasive ventilation. However, the optimal timing for PND initiation is unclear.
Objective:
To investigate the association between PND initiation times and the risk of death or sBPD in VPI.
Design/Methods:
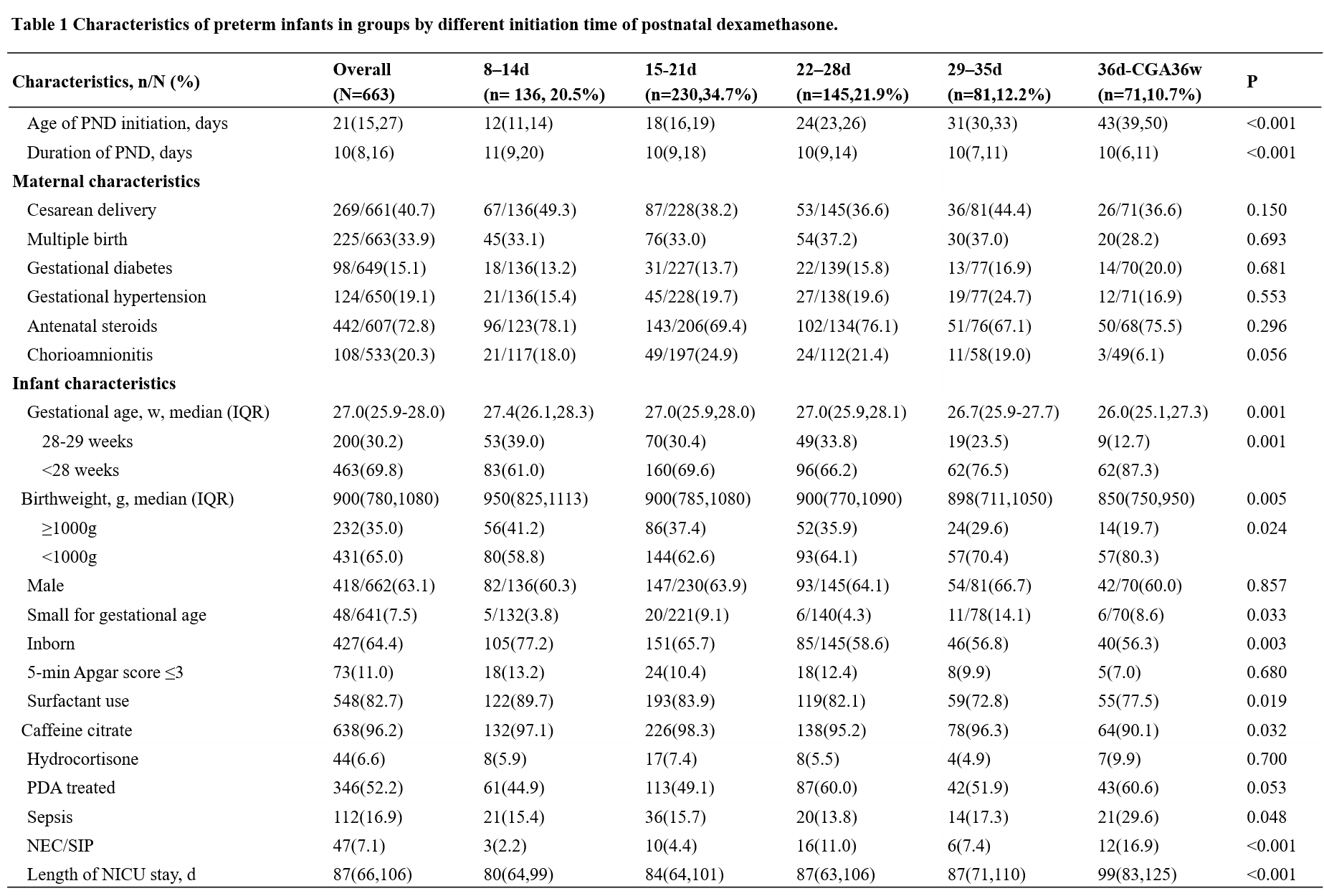
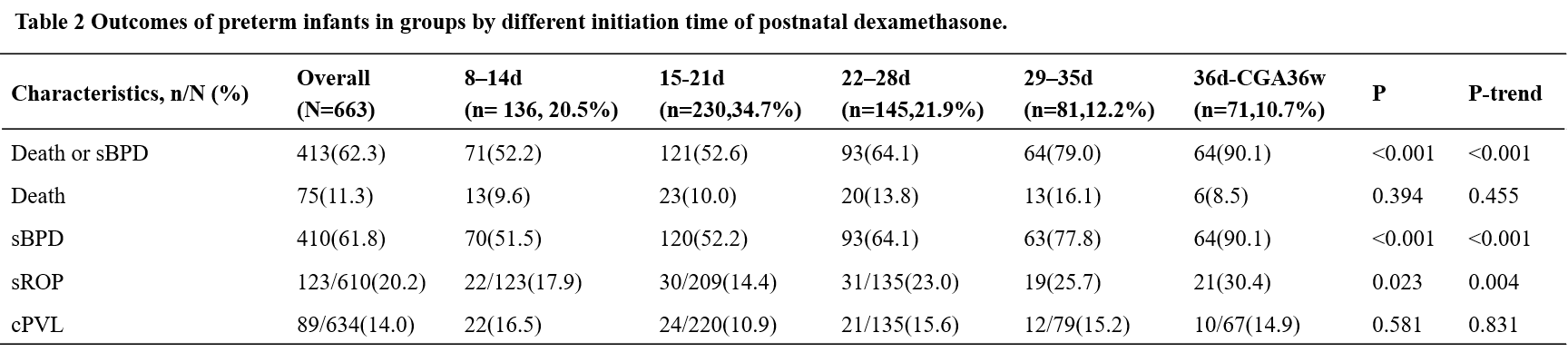
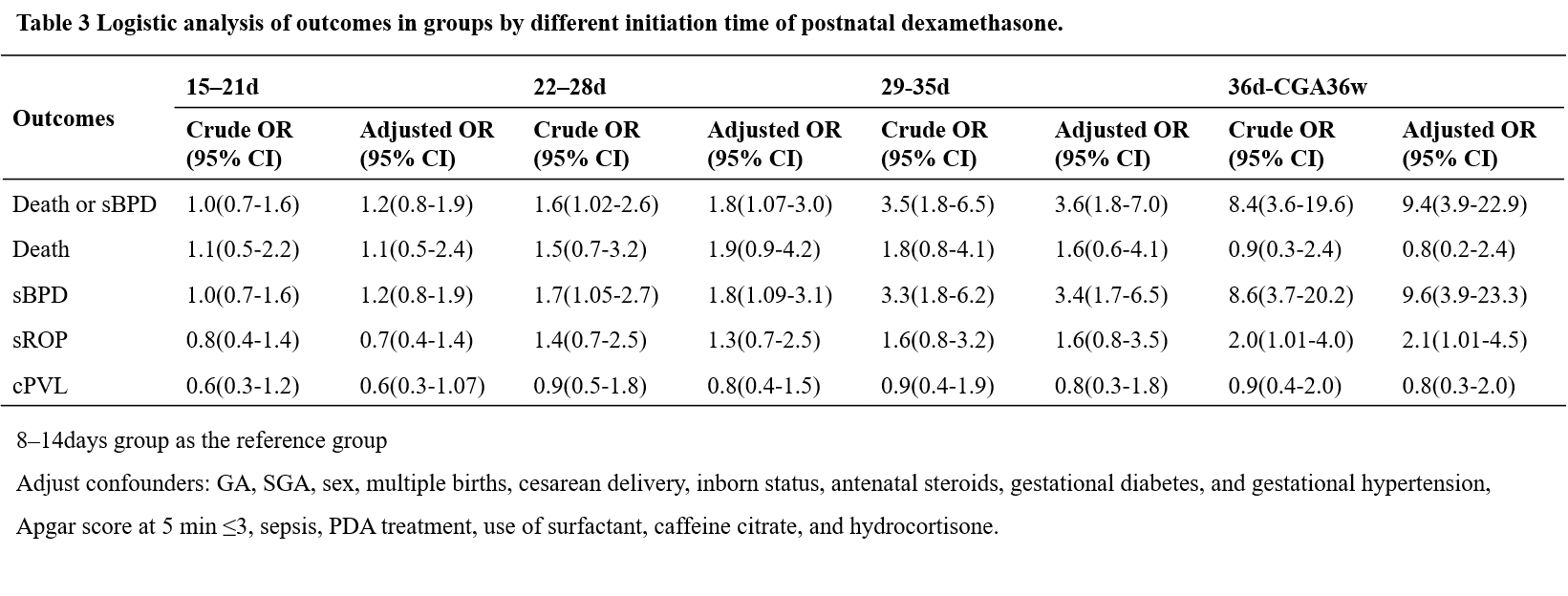
Infants admitted to neonatal intensive care units (NICU) participating in the Chinese Neonatal Network (CHNN) between January 2019 and December 2021, who were born at less than 30 weeks gestational age (GA), required invasive ventilation until at least 7 days of life (DOL), and treated with PND between 8 DOL and 36 weeks corrected GA (cGA) from January 2019 to December 2021, were included in the study. They were categorized into five groups according to PND initiation time (8-14d, 15-21d, 22-28d, 29-35d, 36d-CGA36w). The primary outcome was the incidence of death or sBPD at 36 weeks CGA. Logistic regression analyses were performed to evaluate the association between dexamethasone initiation time and outcomes.
Results:
Among the 3519 VPI who remained on invasive ventilation at DOL of 7 or beyond in the cohort, 663 infants were treated with PND. The overall incidence of death or sBPD was 62.3% (413/663). The incidence of death or sBPD in the 8-14d group (52.2%, n=71/136), was not significantly different from the 15-21d group (52.6%, n=121/230, aOR1.2, 95%CI 0.8-1.9). However, the incidence of death or sBPD increased significantly with PND initiation beyond 21 days: 22-28d group (64.1%, n=93/145, aOR1.8, 95%CI 1.07-3.0), 29-35d group (79.0%, n=64/81, aOR3.6, 95%CI 1.8-7.0) and 36d-CGA36w groups (90.1%, n=64/71, aOR9.4, 95%CI 3.9-23.3). Subgroup analysis by GA demonstrated similar findings.
Conclusion(s):
PND initiation beyond 21 days CGA is associated with increased death or sBPD in preterm infants with prolonged invasive ventilation.