Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
676 - Peri-extubation settings in preterm neonates: A systematic review
Publication Number: 676.443
- YN
Yogesha Karthikere Nagaraj, MD
Fellow
McMaster University, Hamilton Canada
Hamilton, Ontario, Canada
Presenting Author(s)
Background: Peri-extubation settings that optimize successful extubation in preterm neonates are unknown. A summary of published peri-extubation settings and related outcomes may help inform clinical practice and identify knowledge gaps for future research.
Objective: 1) To systematically review and summarize published data on pre- and post-extubation settings; 2) to review and meta-analyze data on association of higher vs. lower pre- and/or post-extubation settings with clinical outcomes, in preterm neonates < 37 weeks’ gestation.
Design/Methods:
Both observational (including case series ≥20 patients) and experimental studies published in English in a peer-reviewed journal were eligible if they reported patient-data on peri-extubation settings (objective 1) or compared two levels of peri-extubation levels with one or more pre-specified clinical outcomes (objective 2). Medline, EMBASE, Cochrane CENTRAL, CINAHL, and Web of Science were searched; following initial screen of titles/abstracts, standardized forms were used by 4 authors independently to extract data from included studies. Risk of bias was determined using a modified Newcastle-Ottawa Scale (for observational studies) and Cochrane Risk of Bias-1 tool (experimental studies). OpenMeta-Analyst [CEBM, Brown University] was used with random effects model for meta-analyses when appropriate, and pooled point-estimates with 95% CIs and I2 (for statistical heterogeneity) were calculated.
Results:
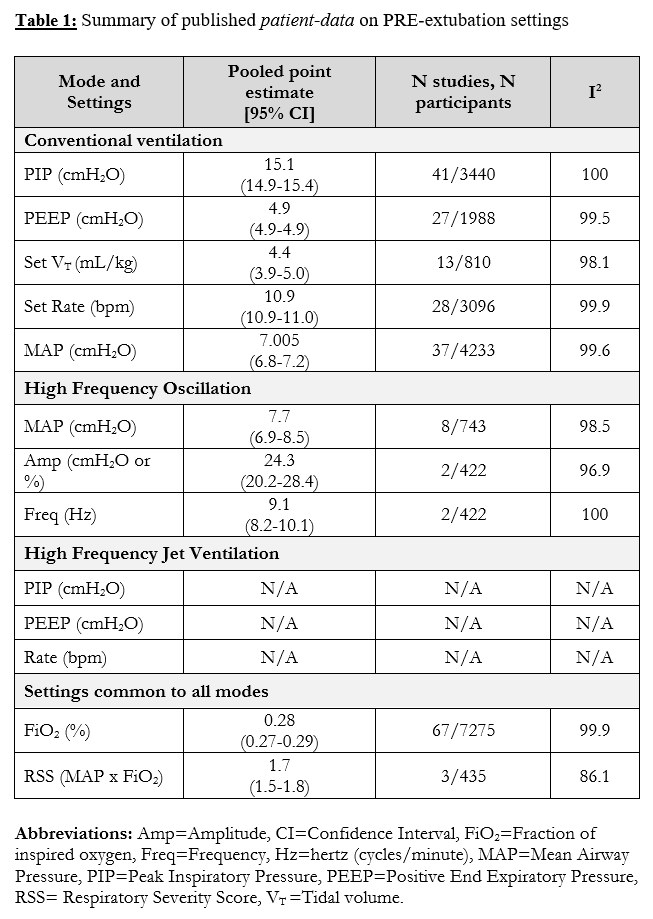
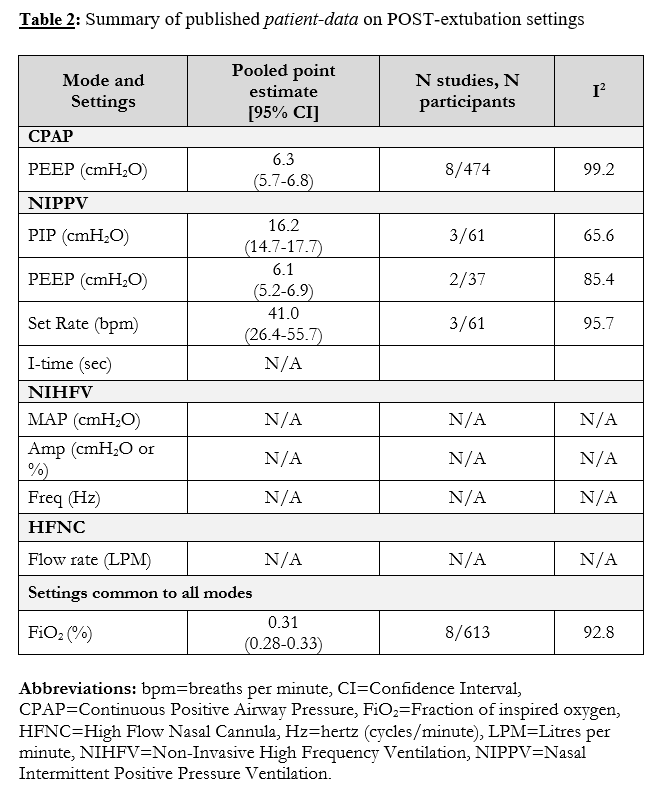
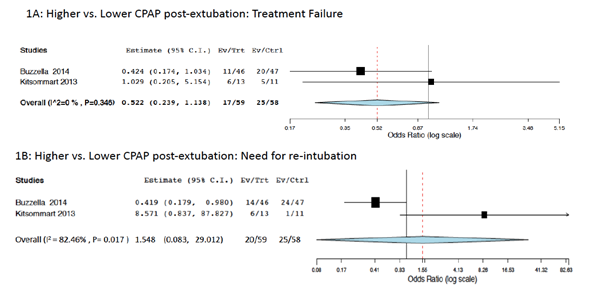
Out of 5283 titles, 355 full-texts were reviewed and 83 included in the review, of which 56 had a low risk of bias. For objective 1, patient-data on pre-extubation settings for conventional ventilation and high frequency oscillation are summarized in Table 1. No studies reported pre-extubation high frequency jet settings. Table 2 summarizes available patient-data on post-extubation settings on continuous positive airway pressure (CPAP) and nasal intermittent positive pressure ventilation, the only modes with available data. All meta-analyses but one had high heterogeneity (I2 >75%). For objective 2, only two studies were identified – both reporting on post-extubation CPAP levels. There were no differences in pooled odds ratios for treatment failure or need for re-intubation with higher vs. lower CPAP (Figure 1). No studies compared pre-extubation settings, or other post-extubation modes.
Conclusion(s): Summary of published patient-data in preterm neonates on peri-extubation settings may help clinicians in their own practices. However, there are limited comparative data on peri-extubation settings that optimize outcomes, which requires further research.