Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 4
102 - Antenatal Vitamin D Treatment Improves Pulmonary Endothelial Cell Function and Response to Proangiogenic Stimuli in a Preeclampsia Model of Bronchopulmonary Dysplasia Associated Pulmonary Hypertension
Publication Number: 102.426

Michael Cookson, MD (he/him/his)
Fellow
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background:
Preeclampsia (PE) is a risk factor for preterm birth and the development of bronchopulmonary dysplasia (BPD) associated pulmonary vascular disease (PVD). We have shown that intraamniotic (IA) exposure to soluble fms-like tyrosine kinase 1 (sFlt-1), an endogenous VEGF antagonist elevated in maternal blood and amniotic fluid in PE, causes abnormal pulmonary vascular development in infant rats. In addition, AN vitamin D (VD; 1,25(OH)2D) treatment improves pulmonary vascular growth after sFlt-1 exposure. However, the direct effects of IA sFlt-1 and AN VD treatment, on pulmonary endothelial cells (PEC) growth and function are unknown.
Objective:
To determine if AN VD treatment preserves PEC growth and tube formation after AN sFlt-1 exposure.
Design/Methods:
Fetal rats were exposed to saline (CTL), recombinant human sFlt-1 (sFlt-1), sFlt-1 + VD, or VD alone via IA injection at E20 and delivered via c-section at E22. At birth, PEC were isolated using immunomagnetic cell separation. In vitro growth and tube formation assays were conducted using standard methods. Growth velocity was assessed over 5 days.
Results:
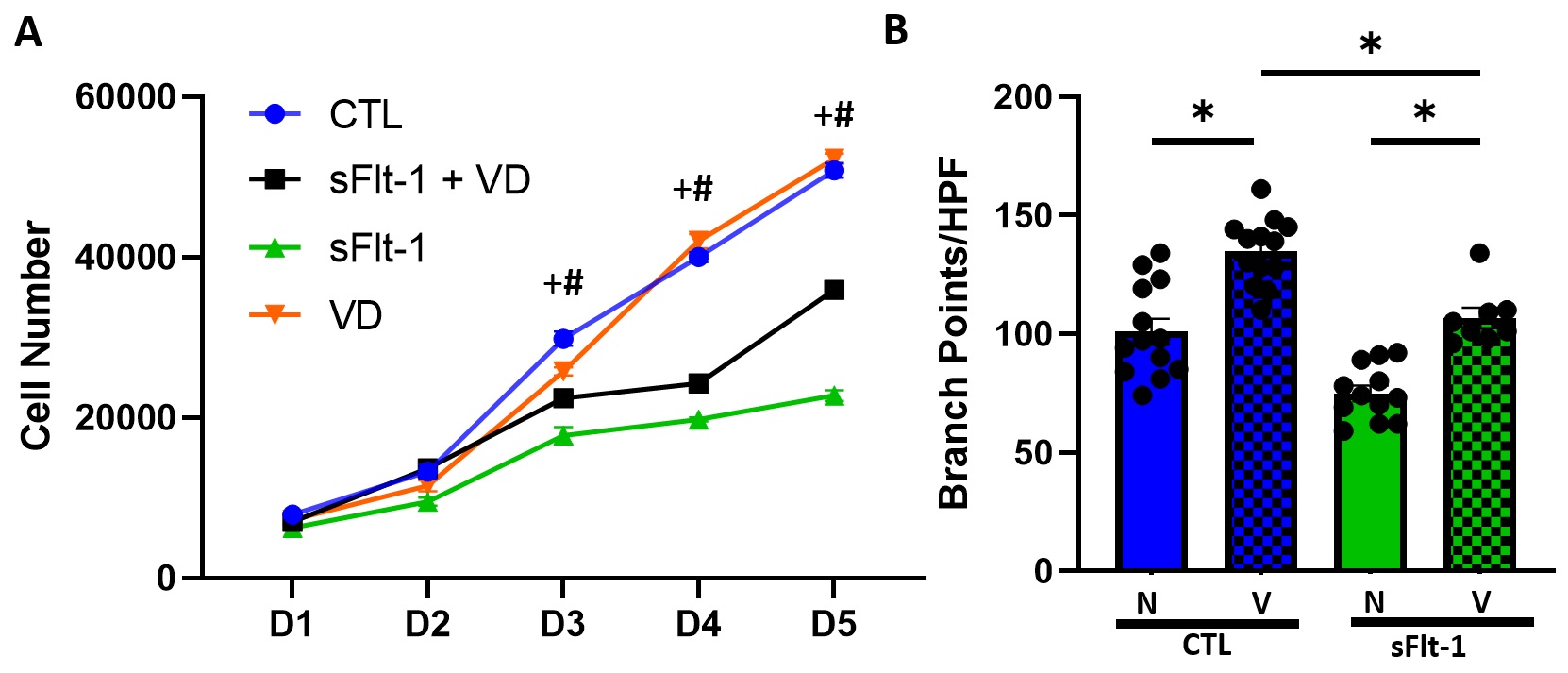
Growth of PEC from sFlt-1 exposed pups was decreased by 40% compared to that of CTL PEC at day 3 (p< 0.05). At day 5, PEC from sFlt-1 exposed pups did not demonstrate further cell growth from day 3, and cell growth decreased by 55% compared to CTL PEC (p< 0.05; Fig. 1A). Growth of PEC from sFlt-1 + VD exposed pups increased by 58% at day 5 compared to PEC from sFlt-1 alone pups (p< 0.05) but was unable to restore growth to that of CTL PEC (sFlt-1 + VD v. CTL; p< 0.05). Growth of PEC from VD alone pups was similar to CTL PEC (p=ns). PEC branching decreased by 25% in sFlt-1 exposed PEC compared to CTL PEC (p< 0.05) (Fig. 1B). PEC branching increased by 26% in sFlt-1 + VD exposed PEC compared to sFlt-1 alone (p< 0.05). VEGF stimulation of CTL PEC increased branching by 30% (p< 0.05). VEGF stimulation of PEC from sFlt-1 exposed pups increased branching by 43% (p< 0.05), similar to that of untreated CTL PEC (p=ns) (Fig. 1B).
Conclusion(s):
AN sFlt-1 exposure decreased PEC tube formation ability and growth velocity. AN VD treatment during sFlt-1 exposure increased both PEC growth velocity and tube formation. AN sFlt-1 exposed PEC were able to respond to VEGF stimulation with increased tube formation similar to that of untreated PEC, but the response was blunted compared to VEGF stimulation of CTL PEC. We speculate that VD treatment of sFlt-1 exposed pups preserves pulmonary vascular development through augmented pro-angiogenic signaling in the endothelial cell.