Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
668 - A quality project to improve 1st attempt successful tracheal intubation in delivery room and neonatal intensive care unit
Publication Number: 668.443
- TN
Tetyana H. Nesterenko, MD, MSHS (she/her/hers)
Clinical Associate Professor of Pediatrics, Neonatologist, Quality Improvement Officer
Cleveland Clinic Children's Hospital
Cleveland, Ohio, United States
Presenting Author(s)
Background:
Tracheal intubation is one of the most common and life-saving procedures in neonatal care. As many as 1-6% of newborns undergo intubation in the delivery room and many others become intubated during NICU course. Intubation is a highly specialized skill, requiring practice and experience in order to gain proficiency. According to the National Emergency Airway Registry for Neonates, first attempt success rate among pediatric residents is 20-30%, and 50-70% among experienced caregivers. Adverse events occur in approximately 20% of intubation encounters, and severe oxygen desaturations occur in up to 50% of encounters.
Objective:
In the population of neonates requiring mechanical ventilation, this project aimed to increase the rate of successful intubation on the 1st attempt by 20%.
Design/Methods:
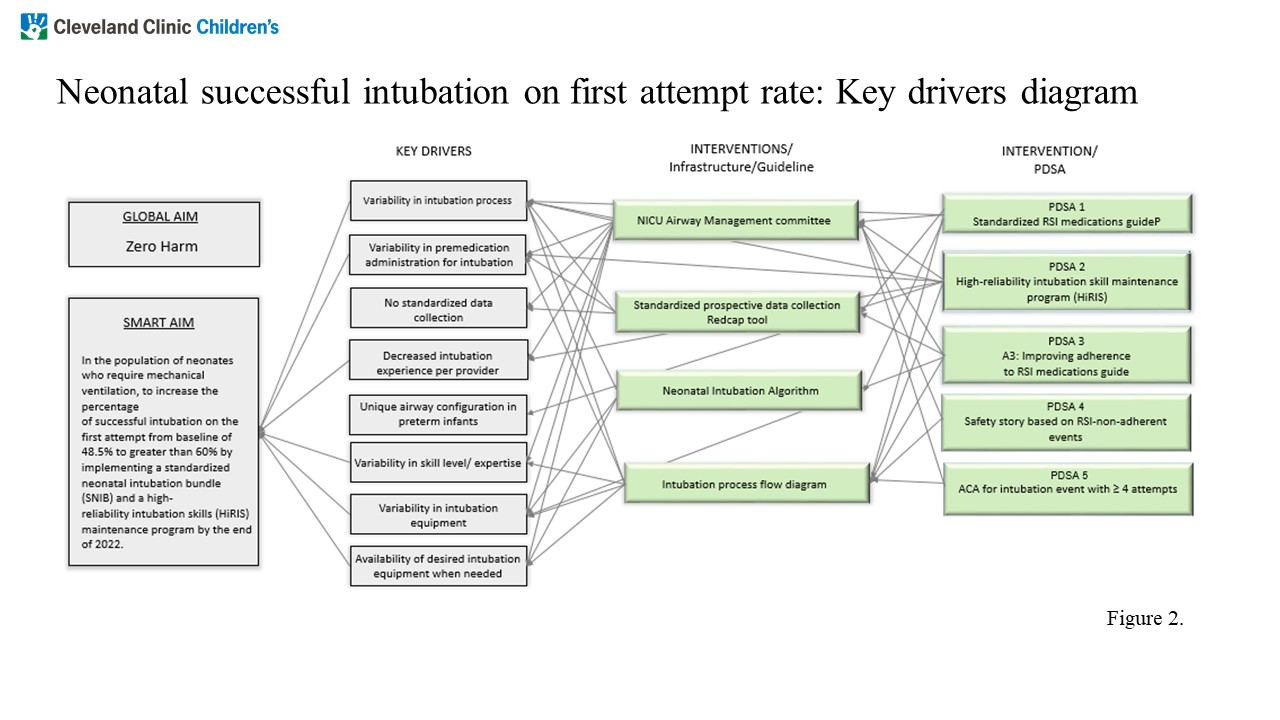
A newly formed NICU Airway Management Committee (NAM) initiated a continuous improvement project at the end of 2020. PDSA 1 cycle, a rapid sequence intubation (RSI) medication guideline implementation, was followed by establishment of structure measures, including a RedCap data collection tool, an intubation process flow diagram, a neonatal intubation algorithm, and a driver diagram (Fig. 1). Baseline success rate was estimated based on retrospective review of intubations over the previous 6 months. A prospective data collection was initiated in November 2020. Intubation was defined as an airway maneuver that starts with the insertion of the laryngoscope into the patient’s mouth and ends with the removal of the device. A high reliability intubation skill (HiRIS) maintenance program was implemented in PDSA cycle 2. The HiRIS program was built on philosophy of deliberate practice among providers and required each provider to complete a monthly intubation simulation by self-assessment to the standard of the checklist. Quarterly, simulations were observed by a member of NAM team to provide an immediate feedback on performance. Adherence to HIRIS program was monitored monthly. PDSA cycle 3 was focused on improving adherence to the use of RSI medication. In PDSA cycle 4, all non-adherent events were reviewed and safety story was presented at the staff meeting.
Results:
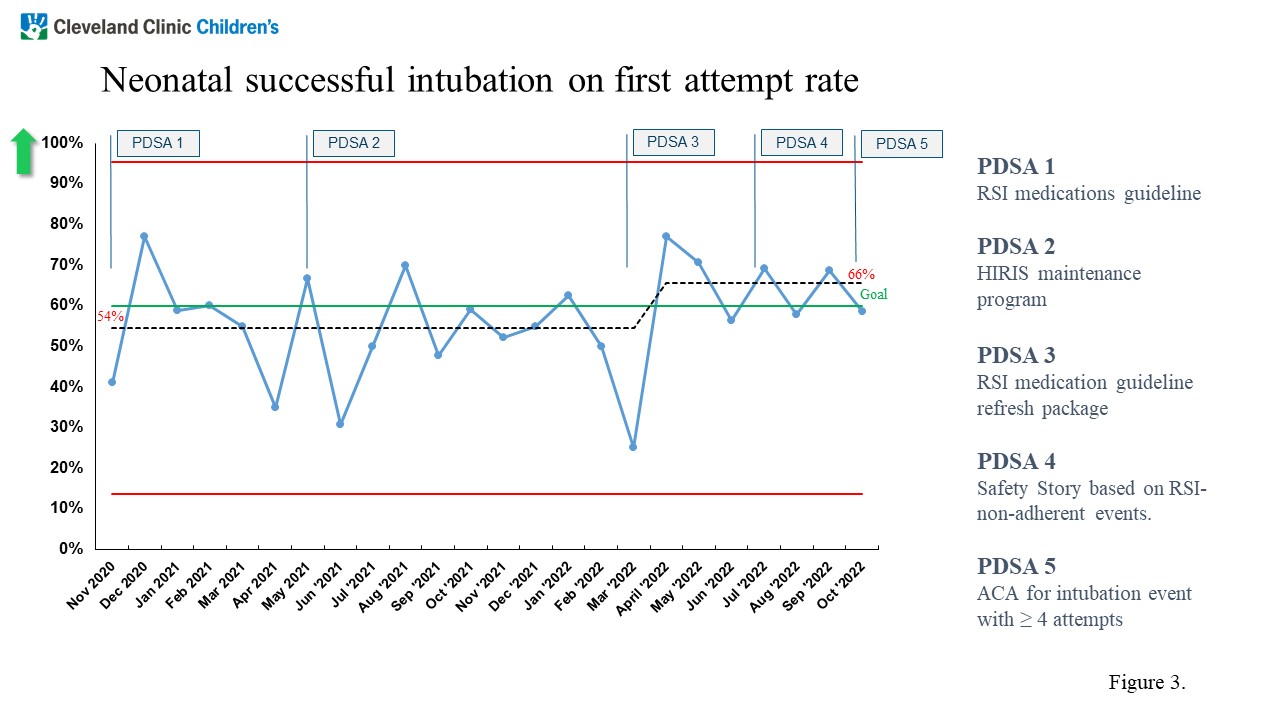
Baseline successful intubation on first attempt was 48.5%. The p-chart (Fig. 2) demonstrates the rate of successful intubation on first attempt during PDSA 1 was 54% that increased to 66% in the current PDSA cycle.
Conclusion(s):
This continuous improvement project resulted in improved success of neonatal intubation on the first attempt. Specific attention to process measures ensures achieving and sustaining high-standard performance.