Injury Prevention
Injury Prevention 2
315 - Epidemiology of Car Seat Tolerance Screening for Infants with Trisomy 21
Publication Number: 315.42

Emily Grace Gerard, MD Candidate (she/her/hers)
Medical Student
University of Maryland School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background:
The American Academy of Pediatrics (AAP) recommends routine pre-discharge car seat tolerance screening (CSTS) for all infants born < 37 weeks gestational age (GA), but also notes that hospitals should develop protocols to include CSTS before discharge for infants at risk of obstructive apnea, bradycardia, or oxygen desaturation other than those born prematurely. Examples include infants with hypotonia and Down syndrome. Previous studies have demonstrated that 10-20% of NICUs and nurseries screen all infants with Trisomy 21 and 30-55% test all those noted to have hypotonia, but no published studies have focused on CSTS outcomes in this high-risk population.
Objective:
To identify incidence and predictors of CSTS failure in a large cohort of infants with Trisomy 21.
Design/Methods:
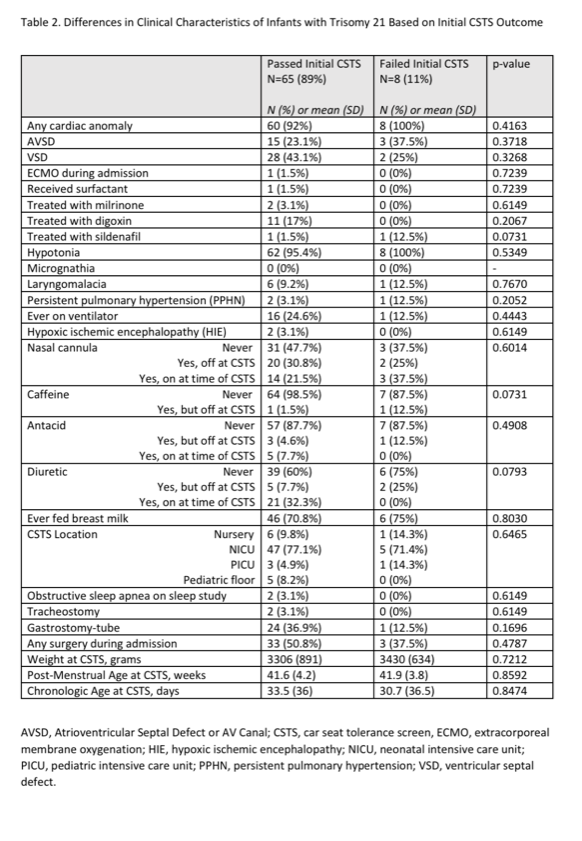
Retrospective medical record review of infants born 2013-2021 diagnosed with Trisomy 21. Identified CSTS failure incidence in this cohort. Collected data on antenatal and clinical factors during admission including birth GA, cardiac and gastrointestinal (GI) comorbidities, and evidence of hypotonia. Performed bivariate analyses comparing clinical and demographic data between infants who did vs. did not undergo CSTS, and between those who passed vs. failed initial CSTS.
Results:
We identified 84 infants with confirmed Trisomy 21 of whom 89% (n=75) had documentation of a pre-discharge CSTS. Ninety-six percent (n=81) were noted to have hypotonia and 20% (n=17) were born prematurely. Of those with documented CSTS results, 11% (n=8) failed their initial CSTS, of which 88% (n=7) were due to desaturation events. Only one (12.5%) of those born prematurely failed their initial CSTS; the remaining 7 (87.5%) CSTS failures were in infants born >=37 weeks GA. In additional, no infants born small for GA (SGA) failed, all CSTS failures were in infants born appropriate for GA (AGA). We found no differences in cardiac, GI, or neurologic diagnoses between those who passed vs. failed initial CSTS.
Conclusion(s):
Infants with Trisomy 21 are at risk for hypotonia, cardiac and GI anomalies, and obstructive apnea, all of which may be exacerbated by the semi-upright car seat position. In fact, we found 11% of subjects in our cohort had unstable respiratory status while in the car seat prior to discharge. These subjects would not have been identified by SGA status or prematurity as the majority were full term and AGA. This demonstrates the importance of including infants with Trisomy 21 in pre-discharge CSTS protocols to allow for appropriate interventions and optimize cardiorespiratory safety in this high-risk group prior to discharge home. .png)