Neonatal Pulmonology
Neonatal Pulmonology 6: Oxygen, Steroids
169 - Optimal timing of antenatal steroids prior to preterm delivery is associated with decreased incidence of bronchopulmonary dysplasia
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 169
Publication Number: 169.438
Publication Number: 169.438
Chanique T. James, University of Miami/Jackson Memorial Hospital, Sunrise, FL, United States; April W. Tan, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States; Mohamed Hamza, Sanford Health - University of North Dakota School of Medicine and Health Sciences, Fargo, ND, United States; Alini Schott, University of miami, Miami, FL, United States; ANA CECILIA. AGUILAR, University of Miami Leonard M. Miller School of Medicine, Miami, Florida 33161, FL, United States; Augusto F. Schmidt, University of Miami Miller School of Medicine, Miami, FL, United States; Nelson Claure, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States

Chanique T. James, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Miami/Jackson Memorial Hospital
Sunrise, Florida, United States
Presenting Author(s)
Background: Antenatal steroids (ANS) reduce the incidence of respiratory distress syndrome (RDS) and mortality in preterm infants, but the effect on bronchopulmonary dysplasia (BPD) is unclear. The lack of effect of ANS on BPD is often empirically attributed to the increased survival of smaller infants with the use of ANS, but there is limited understanding on effects of the timing of ANS administration relative to the preterm birth on BPD.
Objective: To determine the differential effects of the timing of ANS administration relative to birth on respiratory outcomes in a cohort of preterm infants.
Design/Methods: Data from a cohort of infants of 23-30 w gestational age (GA) admitted to the NICU at Holtz Children’s Hospital at the University of Miami/Jackson Memorial Medical Center between Jan/2012 and Dec/2021 were analyzed. ANS was classified into two groups: No ANS or ANS given >7 days before birth (ANS-0) and ANS given within 7 days before birth (ANS-7). ANS consisted of betamethasone-acetate/betamethasone-phosphate 12mg 24h apart. BPD was defined as receiving supplemental oxygen at 36 w postmenstrual age (PMA). Chi-square was used for univariate analysis of categorical variables and Mantel-Haenszel (MH) test was used to estimate the common odds ratio (OR) across GA strata. Multivariate stepwise logistic regression analysis was used to model the association between ANS and BPD.
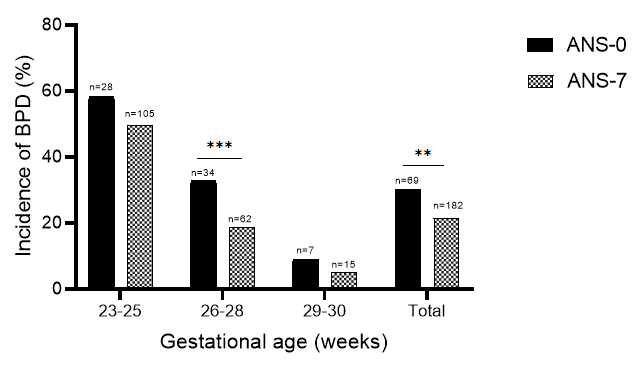
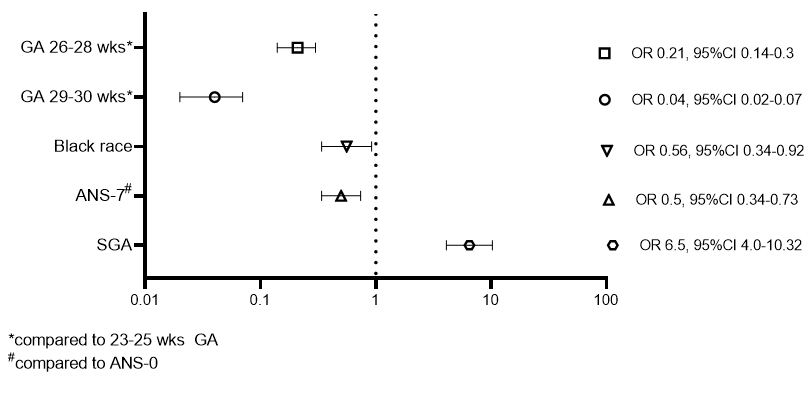
Results: The cohort consisted of 1071 infants alive at 36 w PMA of whom 251 (23%) were classified as having BPD. The incidence of BPD was lower in the ANS-7 compared to the ANS-0 group. This was consistent across GA strata [MH OR (95%CI): 0.555(0.387-0.797)] (Figure 1). Multivariate analysis showed ANS-7 was significantly associated with decreased risk of BPD along with increasing GA and black race, whereas birth weight less than 10% was associated with increased risk of BPD (Figure 2). Histologic chorioamnionitis, pre-eclampsia and Hispanic ethnicity were not associated with BPD risk.
Conclusion(s): In this cohort, ANS administration within 7 days of preterm birth was associated with an independent decreased risk of BPD compared to no ANS or ANS given > 7 days before birth. These findings highlight the impact of timely ANS administration on respiratory outcome and the need for better clinical tools to predict preterm birth and optimize antenatal lung protective therapies.