Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
680 - Validation of Extubation Readiness Tool in Extreme Premature Infants at a Regional Perinatal Center
Publication Number: 680.443

Kavya Rao, MD (she/her/hers)
Assistant Professor of Pediatrics
Jacobs School of Medicine and Biomedical Sciences at University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Background:
In neonates born extremely premature, prolonged invasive mechanical ventilation and failure to extubate are factors associated with increased mortality and morbidities such as bronchopulmonary dysplasia (BPD) requiring prolonged hospitalization leading to poor outcomes. In the absence of accurate tools to assess extubation readiness, many infants fail their extubation attempt which also increases complications. Gupta et al. have developed an online calculator as a tool to assess the chances of extubation success in extremely preterm neonates.
Objective:
Our objective was to a) validate the extubation readiness calculator to predict successful extubation and b) understand if the same factors used in the extubation calculator are applicable to our patient population.
Design/Methods:
Neonates < 29 weeks, who were admitted to our newly built state-of-the-art tertiary NICU over a 2-year period who were on invasive mechanical ventilation, and had an elective extubation attempt within 60 days of age were included. The primary outcome was to validate the extubation success using the calculator, defined as surviving for at least 5 days after extubation, without a need for reintubation. The secondary outcome was to model factors associated with predicting extubation readiness in the calculator. Infants who died or had unplanned extubation were excluded.
Results:
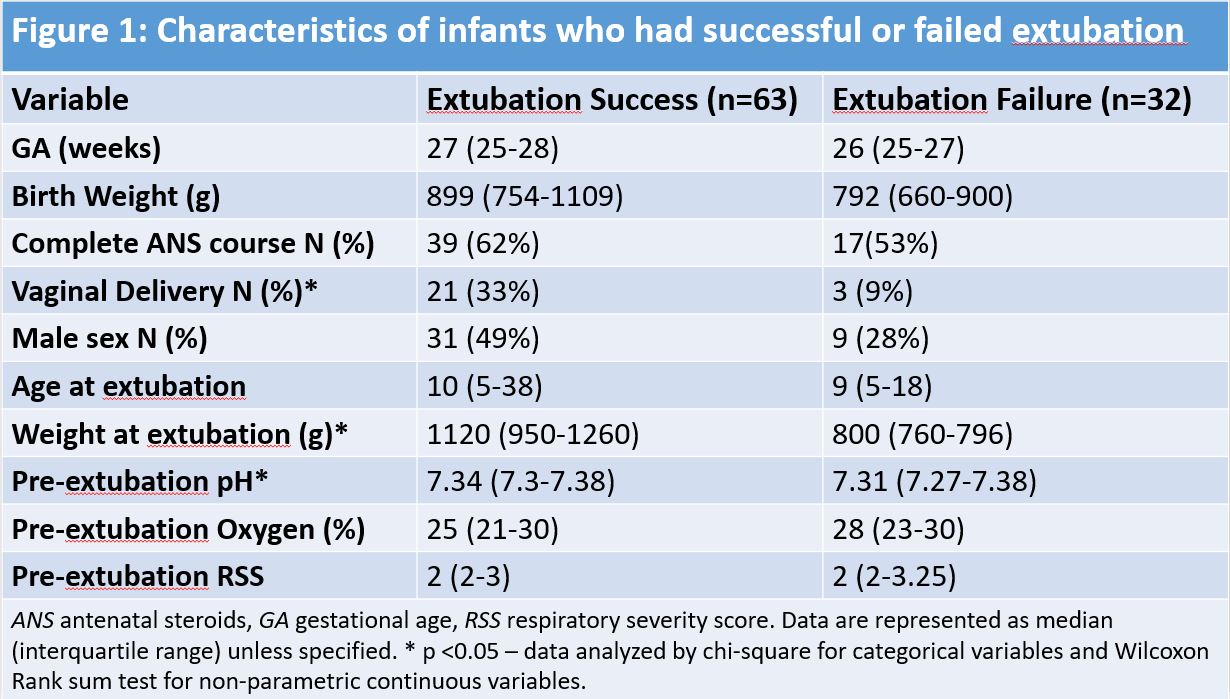
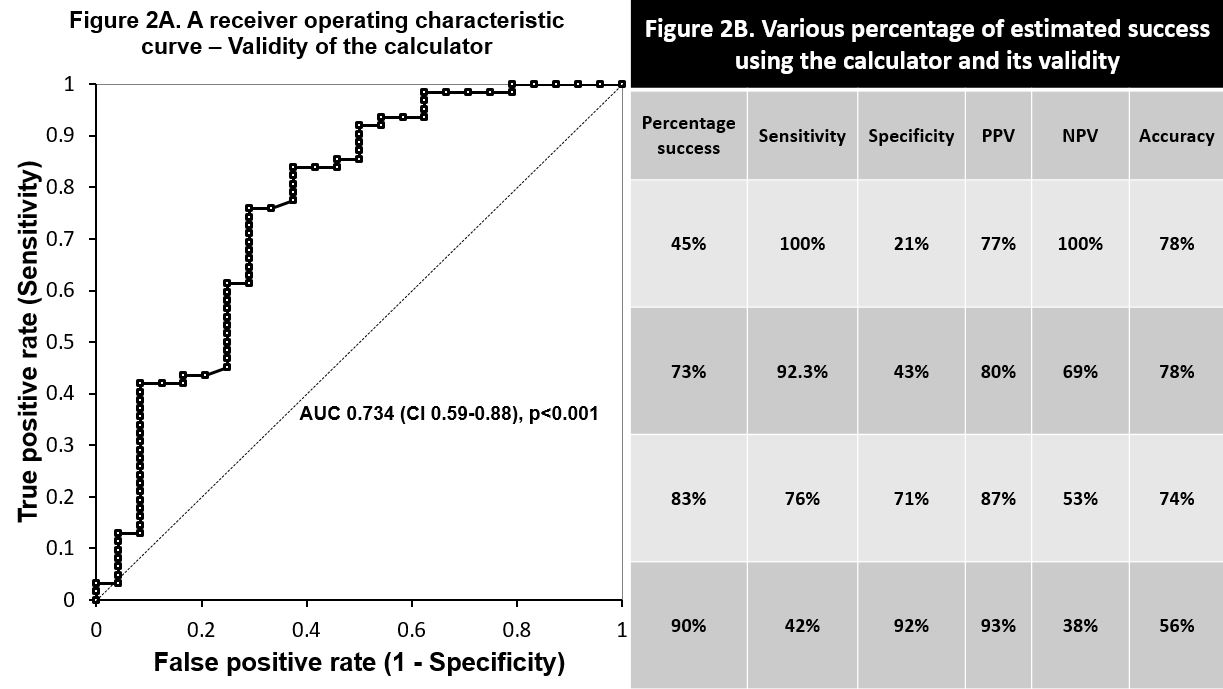
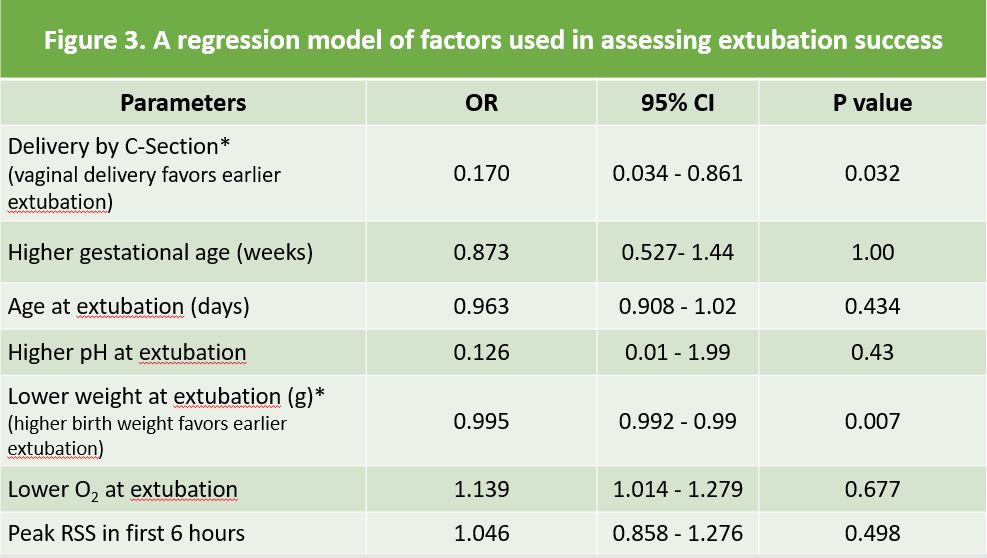
There were 118 infants between 2018 and 2019 who were included. Of the eligible infants, 66% were successfully extubated while 34% of them failed (Fig 1a). The receiver operating characteristic curve (ROC) analysis for the extubation readiness calculator in our cohort was statistically significant with various validity models shown in Figure 1b. 79% had the best sensitivity, specificity, PPV & NPV along with the highest accuracy shown in Figure 1c. At the time of extubation, these infants were larger, born at higher gestation, and had higher pre-extubation pH and lower oxygen (O2) requirements than those who failed extubation (Fig 2). Vaginal delivery and higher birth weight were statistically significant in our model to predict extubation readiness favoring extubation success.
Conclusion(s): In our cohort that included data for 2 years, the calculator was validated in infants who were extubated with variable chances of success rate. This tool could provide quantitative evidence in helping predict significant improvements in extubation outcomes in the extreme preterm population. With evolving changes in ventilation practices, we intend to create a BPD bundle to assess other factors that could influence early extubation and its effect on BPD and mortality.